Ulcerative colitis (UC) is a chronic inflammatory disease of the colon that affects millions worldwide. This guide offers an in‐depth look at its definition, alternative names, causes, symptoms, diagnostic tests, treatment options, available support groups, prognosis, possible complications, when to seek medical attention, and preventive measures. The information presented here is based on up‐to‐date and credible sources from leading institutions such as the Mayo Clinic, Penn Medicine, and the National Institutes of Health, among others mayoclinic.org, pennmedicine.org, medlineplus.gov.
1. Definition and Alternative Names
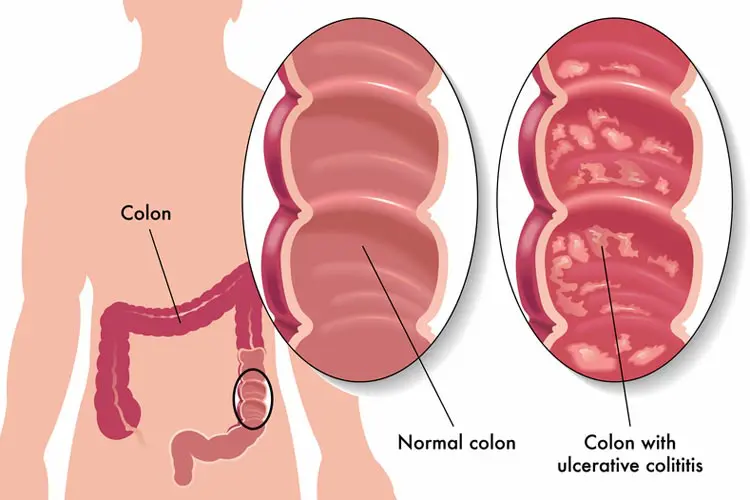
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes chronic inflammation and ulceration of the colon and rectum. Unlike Crohn’s disease—which can affect any part of the gastrointestinal (GI) tract—UC is limited to the large intestine. The disease is characterized by recurring episodes of active inflammation (flares) followed by periods of remission.
Alternative Names
Ulcerative colitis is sometimes referred to by other names, including:
- Colitis
- Inflammatory bowel disease – ulcerative colitis
- Ulcerative proctitis (when the inflammation is confined to the rectum)
- Proctosigmoiditis (when the rectum and sigmoid colon are involved)
These terms are used depending on the extent and location of the disease.
2. Causes and Risk Factors
Although the precise cause of ulcerative colitis remains unknown, research suggests that a combination of genetic, environmental, and immune system factors contribute to its development.
2.1 Genetic Factors
A family history of IBD increases the risk of developing ulcerative colitis. Studies indicate that a first‐degree relative with UC can raise the risk several fold. Researchers have identified various genetic markers and genomic regions (such as those on chromosomes 6 and 1) that may predispose individuals to the disease pennmedicine.org.
2.2 Immune System Dysregulation
UC is considered an autoimmune disorder. In susceptible individuals, the immune system mistakenly attacks the colon’s lining, causing chronic inflammation. This abnormal immune response may be triggered by:
- An inappropriate reaction to the normal gut microbiota.
- A malfunction in the regulatory pathways that normally suppress inflammation.
2.3 Environmental Factors
Environmental elements also play a significant role. Some factors that have been implicated include:
- Diet: A Western diet rich in processed foods may contribute to an increased incidence of UC.
- Smoking: Interestingly, while smoking is a known risk factor for Crohn’s disease, it may have a protective effect in ulcerative colitis. However, the risks of smoking far outweigh any potential benefits.
- Hygiene Hypothesis: Reduced exposure to certain bacteria or parasites during early life (due to high standards of cleanliness) may influence the immune system and contribute to UC.
- Appendectomy: Some studies suggest that removal of the appendix early in life may lower the risk of developing UC.
Together, these factors set the stage for the onset of UC in individuals who are genetically predisposed.
3. Symptoms of Ulcerative Colitis
The hallmark of ulcerative colitis is inflammation of the colon, which leads to a range of symptoms that can vary in intensity. Symptoms may be mild and intermittent during remission or severe and debilitating during flare-ups.
3.1 Gastrointestinal Symptoms
The primary symptoms related to the colon include:
- Diarrhea: One of the most common symptoms, diarrhea in UC is often frequent and may be mixed with blood and mucus. This is due to the ulcerated, inflamed lining of the colon.
- Abdominal Pain and Cramping: Pain usually occurs in the lower abdomen, correlating with the areas of active inflammation. Cramps are common during bowel movements.
- Rectal Bleeding: Bleeding is a frequent sign of mucosal ulceration. Patients may notice blood in their stool or on toilet paper.
- Urgency and Tenesmus: Many individuals feel an urgent need to have a bowel movement. Tenesmus, the sensation of incomplete evacuation despite frequent bowel movements, is also common.
- Weight Loss: Ongoing inflammation and malabsorption can lead to unintended weight loss.
- Fatigue: Chronic inflammation and nutrient loss often result in tiredness and reduced energy.
3.2 Extraintestinal Manifestations
While ulcerative colitis primarily affects the colon, it can also have systemic effects that impact other parts of the body:
- Joint Pain (Arthralgia): Some patients experience arthritis or arthralgia, particularly in the large joints.
- Skin Conditions: Conditions such as erythema nodosum (tender red nodules, usually on the shins) and pyoderma gangrenosum (painful skin ulcers) can occur.
- Eye Inflammation: Uveitis, episcleritis, and scleritis are possible, which may cause redness, pain, and blurred vision.
- Liver Disease: Although less common, primary sclerosing cholangitis (PSC), a disease affecting the bile ducts, is associated with UC.
- Oral Lesions: Mouth ulcers (aphthous stomatitis) may also appear in some patients.
3.3 Variation by Disease Extent
The clinical presentation often depends on the extent of colon involvement:
- Proctitis: Inflammation confined to the rectum may lead to rectal pain, bleeding, and urgency.
- Left-Sided Colitis: Involvement from the rectum to the descending colon usually presents with more pronounced abdominal pain and diarrhea.
- Pancolitis: When the entire colon is affected, symptoms are more severe, with frequent, voluminous bloody diarrhea, significant weight loss, and systemic symptoms such as fever.
3.4 Symptom Fluctuation
A key characteristic of UC is its relapsing-remitting course. During remission, many patients may experience few or no symptoms, while flare-ups can be unpredictable and vary from mild exacerbations to fulminant colitis requiring hospitalization.
4. Diagnostic Exams and Tests
Accurate diagnosis of ulcerative colitis is essential for effective management. The diagnostic process typically involves a combination of history-taking, physical examination, laboratory tests, and imaging studies.
4.1 Medical History and Physical Examination
A detailed medical history is crucial and should focus on:
- Duration and nature of symptoms (diarrhea, abdominal pain, rectal bleeding)
- Family history of IBD or other autoimmune disorders
- Recent infections, medication use, and lifestyle factors
A thorough physical exam may reveal signs of anemia, weight loss, abdominal tenderness, and extraintestinal manifestations (such as joint swelling or skin lesions).
4.2 Laboratory Tests
Blood and stool tests help to assess inflammation, rule out infections, and evaluate for complications:
- Complete Blood Count (CBC): May show anemia due to chronic blood loss and inflammation.
- C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Elevated levels indicate systemic inflammation.
- Stool Studies: These tests can exclude infectious causes of diarrhea and measure markers such as fecal calprotectin or lactoferrin, which are elevated in IBD.
- Liver Function Tests: To screen for PSC, especially in patients with long-standing or extensive disease.
4.3 Endoscopic Procedures
Endoscopy is the gold standard for diagnosing UC:
- Colonoscopy: This procedure allows direct visualization of the entire colon and rectum. Findings in UC include a continuous pattern of inflammation, loss of the normal vascular pattern, mucosal friability, and ulcerations. Biopsies taken during colonoscopy help confirm the diagnosis histologically.
- Flexible Sigmoidoscopy: Often used in patients with severe symptoms or those at risk for complications, as it is less invasive. However, it may miss disease in the proximal colon if the disease is more extensive.
4.4 Imaging Studies
While not always necessary, imaging may be used in specific cases:
- Abdominal X-ray: Can be useful for detecting complications such as toxic megacolon or perforation.
- CT Scan or MRI: These imaging modalities may help assess the extent of inflammation, complications, or when a complete colonoscopy is contraindicated.
4.5 Histopathologic Examination
Biopsy samples obtained during endoscopy reveal:
- Crypt Abscesses: Collections of neutrophils within the glandular crypts.
- Mucosal Ulceration and Erosion: Reflecting the damage from chronic inflammation.
- Architectural Distortion: Chronic changes in the glandular structure of the colon.
Histology confirms that the inflammation is confined to the mucosal layer, distinguishing UC from Crohn’s disease, where inflammation is transmural
5. Treatment Options
The treatment of ulcerative colitis is aimed at inducing remission during flare-ups and maintaining long-term remission. Treatment plans are individualized based on the severity and extent of the disease, as well as the patient’s overall health.
5.1 Medications
A range of medications is available to manage UC:
5.1.1 Aminosalicylates (5-ASA)
These are the first-line treatments for mild to moderate ulcerative colitis. They work by reducing inflammation directly in the colon.
- Mesalazine (Mesalamine): Available in various formulations (oral tablets, enemas, suppositories) and marketed under brand names such as Asacol, Lialda, and Pentasa.
- Sulfasalazine: Decomposes in the intestine to release 5-ASA and an antibiotic component.
Aminosalicylates are effective both for inducing remission and as maintenance therapy, although side effects (e.g., nausea, headache) must be monitored.
5.1.2 Corticosteroids
These drugs are used to control acute flare-ups due to their potent anti-inflammatory effects.
- Prednisone, Hydrocortisone, and Methylprednisolone: Typically used for short-term control as they are not suitable for long-term therapy because of their side-effect profile (e.g., weight gain, osteoporosis, Cushing’s syndrome).
- Budesonide: A corticosteroid with high first-pass metabolism that minimizes systemic side effects.
Corticosteroids help achieve rapid symptom relief but should be tapered off once remission is induced.
5.1.3 Immunomodulators
These drugs work by suppressing the immune system to reduce chronic inflammation.
- Azathioprine and 6-Mercaptopurine: Often used for maintenance therapy, particularly in patients who are steroid-dependent.
- Methotrexate: May be used in selected patients, especially those with concomitant arthritis.
Regular monitoring is required due to the risk of bone marrow suppression and liver toxicity.
5.1.4 Biologic Therapies
Biologics target specific components of the immune system and have revolutionized the treatment of moderate to severe ulcerative colitis.
- TNF Inhibitors (e.g., Infliximab, Adalimumab, Golimumab): Block tumor necrosis factor (TNF), a key cytokine in the inflammatory process.
- Integrin Receptor Antagonists (e.g., Vedolizumab): Block the migration of inflammatory cells to the gut.
- Janus Kinase (JAK) Inhibitors (e.g., Tofacitinib): Target intracellular signaling pathways involved in inflammation.
Biologics are generally reserved for patients who do not respond adequately to conventional therapies
.
5.1.5 Targeted Synthetic Small Molecules
Newer agents, such as tofacitinib, work by modulating specific pathways (JAK-STAT) that drive inflammation. These drugs offer oral administration and are an alternative for patients who do not tolerate or respond to biologics.
5.2 Surgical Options
Surgery is typically considered when medical therapy fails or in the presence of complications such as massive hemorrhage, toxic megacolon, or cancer.
- Proctocolectomy: Removal of the colon and rectum is considered curative for ulcerative colitis, though it does not reverse extraintestinal manifestations.
- Ileal Pouch-Anal Anastomosis (IPAA): After colectomy, a pouch is constructed from the small intestine and connected to the anus to preserve bowel continence.
Surgical decisions are made on a case-by-case basis and are typically reserved for severe or refractory cases.
5.3 Dietary and Lifestyle Modifications
Although no specific diet has been proven to cure UC, dietary modifications can help manage symptoms:
- Low-Residue Diet: May reduce bowel frequency during flare-ups.
- Avoidance of Trigger Foods: Some patients find that spicy foods, dairy (if lactose intolerant), and high-fiber foods exacerbate symptoms.
- Nutritional Support: Supplements (e.g., iron, vitamin D) may be necessary due to malabsorption and chronic blood loss.
5.4 Complementary and Alternative Therapies
Many patients explore additional strategies to manage stress and improve quality of life:
- Probiotics: Supplementation may help restore the natural balance of gut bacteria and has shown some promise in inducing remission in UC.
- Mind-Body Techniques: Stress reduction through mindfulness, yoga, or cognitive behavioral therapy can alleviate symptom severity.
- Acupuncture: Although evidence is mixed, some patients report symptomatic relief.
It is essential to discuss any complementary approaches with a healthcare provider.
6. Available Support Groups and Resources
Living with ulcerative colitis can be challenging both physically and emotionally. Fortunately, many support groups and organizations offer assistance, resources, and community connections.
6.1 National and International Organizations
- Crohn’s & Colitis Foundation: A leading organization providing educational resources, patient support networks, and advocacy programs in the United States.
- Crohn’s & Colitis Australia: Offers support groups, information, and advocacy for people in Australia, where IBD prevalence is high.
- European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA): Connects patients across Europe to share experiences and access support.
6.2 Online Forums and Communities
- Mayo Clinic Connect: An online community where patients share their experiences and offer support.
- Reddit (r/UlcerativeColitis and r/IBD): Popular forums for personal stories, tips, and emotional support.
- Facebook Groups: Many regional and international groups exist where members can share advice and offer mutual support.
6.3 Local Support Groups and Counseling
Many hospitals and clinics offer support groups, counseling services, and educational workshops. Patients are encouraged to ask their gastroenterologists or primary care providers for referrals to local resources.
7. Prognosis and Disease Course
Ulcerative colitis is a lifelong condition, but the disease course varies widely among individuals.
7.1 Remission and Flare-Ups
- Remission: Many patients experience periods of remission during which symptoms may be minimal or absent. Maintenance therapy is crucial to prolong these periods.
- Flares: Episodes of increased inflammation can cause a return of symptoms. These flares may be unpredictable and range from mild to severe.
7.2 Long-Term Outlook
- Quality of Life: With appropriate treatment, many patients lead active lives. However, persistent symptoms can impact daily functioning.
- Risk of Colon Cancer: The risk of developing colorectal cancer increases with the duration and extent of the disease. Regular colonoscopic surveillance is recommended, particularly after 8–10 years of disease activity.
- Extraintestinal Manifestations: Some patients may continue to experience complications outside the GI tract, which require separate management.
7.3 Factors Affecting Prognosis
Prognostic factors include:
- Age at Onset: Younger patients may have a more aggressive disease course.
- Extent of Disease: Pancolitis generally carries a worse prognosis than limited proctitis.
- Response to Therapy: Early response to treatment is a good prognostic indicator.
- Nutritional Status: Malnutrition can complicate the disease course and affect overall outcomes.
Ongoing research aims to identify biomarkers that could better predict disease progression and response to therapy ncbi.nlm.nih.gov.
8. Possible Complications
Without proper management, ulcerative colitis can lead to several complications, some of which may be life-threatening.
8.1 Gastrointestinal Complications
- Toxic Megacolon: A severe complication where the colon dilates dangerously, potentially leading to perforation and sepsis.
- Perforation: The ulcerated colon may develop holes, allowing intestinal contents to leak into the abdominal cavity—a surgical emergency.
- Severe Bleeding: Chronic or acute blood loss can lead to anemia and may require transfusion.
- Strictures and Pseudopolyps: Chronic inflammation can result in scarring (strictures) and the formation of pseudopolyps, which are benign but may complicate the disease.
8.2 Increased Cancer Risk
Long-standing ulcerative colitis, especially pancolitis, increases the risk of colorectal cancer. Surveillance colonoscopies are essential to detect precancerous changes early.
8.3 Extraintestinal Complications
- Arthritis: Inflammation of the joints can range from mild pain to severe arthritis.
- Ocular Inflammation: Conditions like uveitis and episcleritis can impair vision.
- Skin Conditions: Erythema nodosum and pyoderma gangrenosum are examples of skin complications.
- Liver Disorders: Primary sclerosing cholangitis (PSC) is a significant complication that affects the bile ducts and increases cancer risk.
- Bone Density Loss: Long-term steroid use can lead to osteoporosis.
Early recognition and proactive management of these complications are key to preventing long-term morbidity.
9. Indications for Seeking Medical Attention
It is crucial to recognize when symptoms warrant prompt medical evaluation. Patients should seek immediate medical care if they experience:
- Severe Abdominal Pain: Especially if accompanied by high fever or signs of peritonitis (e.g., guarding, rebound tenderness).
- Persistent or Worsening Diarrhea: Particularly if it is bloody and accompanied by signs of dehydration.
- Rapid Weight Loss: Unexplained and significant loss of weight may indicate severe inflammation or malabsorption.
- Symptoms of Toxic Megacolon: Such as extreme abdominal distension, fever, rapid heart rate, and confusion.
- Signs of Anemia: Including dizziness, fatigue, pale skin, or shortness of breath.
- New Extraintestinal Symptoms: Sudden joint pain, eye redness, or skin lesions should prompt evaluation.
- Uncontrolled Symptoms Despite Medication: If current therapies do not seem to be effective or if symptoms are worsening.
Recognizing these red flags can prevent complications and allow for timely adjustments in treatment.
10. Preventive Measures and Lifestyle Modifications
While ulcerative colitis cannot be prevented entirely, certain strategies can reduce the frequency and severity of flares and improve overall well‐being.
10.1 Medication Adherence
Adherence to prescribed medications is crucial to maintaining remission and preventing flares. Skipping doses or discontinuing treatment without consulting a healthcare provider can lead to a relapse.
10.2 Dietary Management
- Balanced Diet: Focus on a balanced diet rich in lean proteins, fruits, vegetables, and whole grains. Adjust the fiber content during flare-ups as needed.
- Food Diary: Keeping a record of food intake and symptoms can help identify personal trigger foods.
- Nutritional Supplements: In cases of malabsorption or chronic blood loss, supplements such as iron, vitamin D, and B vitamins may be necessary.
- Avoiding Irritants: Limiting spicy foods, caffeine, and alcohol may help reduce gastrointestinal irritation.
10.3 Stress Reduction
Stress does not cause ulcerative colitis but can trigger flares. Incorporating stress management techniques such as:
- Mindfulness Meditation
- Yoga
- Regular Physical Activity
- Counseling or Therapy
can improve both mental health and disease control.
10.4 Regular Monitoring and Follow-Up
- Routine Medical Check-Ups: Regular follow-ups with your gastroenterologist are essential to monitor disease activity and adjust treatments.
- Screening for Complications: Periodic colonoscopies and laboratory tests help detect complications, such as colon cancer or nutrient deficiencies, early.
- Vaccinations: Staying current on vaccinations (e.g., influenza, pneumonia) is important, especially for patients on immunosuppressive therapy.
10.5 Lifestyle Changes
- Smoking Cessation: Although smoking may have a paradoxical protective effect in UC, its overall health risks make cessation essential.
- Regular Exercise: Moderate physical activity supports overall health and can help maintain a healthy weight.
- Sleep Hygiene: Ensuring adequate sleep helps manage stress and supports immune function.
Adopting these preventive measures can empower patients to take control of their health and potentially reduce the frequency of flare-ups.
11. References and Credible Medical Sources
Below is a list of some key references that underpin the information in this article. These sources have been carefully selected for their credibility and recency:
- Mayo Clinic. “Ulcerative Colitis – Symptoms & Causes.” Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
- Penn Medicine. “Ulcerative Colitis – Definition, Symptoms, and Diagnosis.” Penn Medicine, https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/ulcerative-colitis
- MedlinePlus. “Ulcerative Colitis.” U.S. National Library of Medicine, https://medlineplus.gov/ency/article/000250.htm
- NCBI Bookshelf – StatPearls. “Ulcerative Colitis.” National Institutes of Health, https://www.ncbi.nlm.nih.gov/books/NBK459282/
- Merck Manuals. “Ulcerative Colitis.” Merck Manuals Consumer Version, https://www.merckmanuals.com/home/digestive-disorders/inflammatory-bowel-diseases-ibd/ulcerative-colitis
- Crohn’s & Colitis Foundation. “Understanding Ulcerative Colitis.” Crohn’s & Colitis Foundation, https://www.crohnscolitisfoundation.org
- Additional peer-reviewed articles and consensus guidelines from journals such as The Lancet, The American Journal of Gastroenterology, and Gut have also informed this article.