1. Definition and Alternative Names
1.1 What Is Respiratory (Pulmonary) Embolism?
A respiratory embolism—more commonly known as a pulmonary embolism (PE)—occurs when an embolus, most often a blood clot, travels through the bloodstream and lodges in one of the pulmonary arteries, obstructing blood flow to part of the lung. This blockage impairs oxygen transfer, raises pulmonary arterial pressure, and forces the right side of the heart to work harder to pump blood through the narrowed vessels.
1.2 Alternative Names
Because of its varied origins and presentations, pulmonary embolism is known by several names:
- Pulmonary Embolism (PE): The most widely used term, describing an embolus lodged in a pulmonary artery.
- Respiratory Embolism: A less common term emphasizing the impact on the respiratory system.
- Pulmonary Arterial Embolism: Occasionally used to specify that the embolus is in the pulmonary arterial circulation.
- Embolic Lung Disease: A broader term that may also refer to embolization of other materials (e.g., fat, air, amniotic fluid) into the pulmonary circulation, though blood clots account for the vast majority.
Understanding these terms is important as they underscore that while the underlying event—a blockage in the lung’s vasculature—is the same, the source of the embolus (typically a deep vein thrombosis) and its clinical implications can vary.
2. Causes and Risk Factors
2.1 Causes of Respiratory (Pulmonary) Embolism
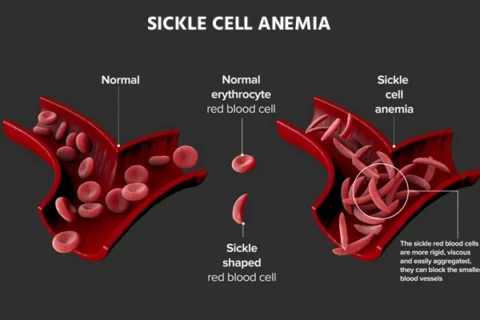
Pulmonary embolism is most commonly caused by a blood clot that forms in the deep veins of the legs or pelvis (a condition known as deep vein thrombosis, or DVT). When part or all of the clot dislodges, it travels through the venous system, passes through the right side of the heart, and becomes lodged in the pulmonary arteries. However, emboli can also originate from other sources, including:
- Fat Emboli: Often occur after fractures of long bones or orthopedic surgery.
- Air Emboli: Can result from invasive procedures, such as central venous catheter placement.
- Amniotic Fluid Emboli: Rare but life-threatening events during labor or postpartum.
- Septic Emboli: Caused by infections that result in fragments of infected material traveling to the lungs.
While blood clots (thrombi) are the most frequent cause of pulmonary embolism, these other types underscore that an embolus in the lung may originate from various materials.
2.2 Risk Factors
Risk factors for pulmonary embolism can be grouped into genetic and acquired factors. Understanding these factors is crucial for prevention and early diagnosis:
2.2.1 Genetic and Inherited Risk Factors
- Inherited Thrombophilias: Genetic conditions that increase the tendency for blood to clot, such as Factor V Leiden mutation, prothrombin gene mutation (G20210A), protein C deficiency, protein S deficiency, and antithrombin deficiency.
- Family History: A personal or family history of deep vein thrombosis or pulmonary embolism increases the risk.
2.2.2 Acquired Risk Factors
- Prolonged Immobilization: Extended periods of bed rest due to surgery, illness, or long-haul travel can slow blood flow in the legs, leading to clot formation.
- Recent Surgery or Trauma: Particularly orthopedic surgery (e.g., hip or knee replacement) increases clot risk due to vascular injury and immobility.
- Pregnancy and Postpartum Period: Hormonal changes and physical compression from the growing uterus, as well as postpartum immobility, contribute to increased risk.
- Cancer: Certain cancers, especially those of the pancreas, lung, colon, and ovary, as well as treatments like chemotherapy, can increase the likelihood of clot formation.
- Hormone Replacement Therapy and Oral Contraceptives: Estrogen-containing medications can promote blood clotting.
- Obesity: Excess body weight is associated with increased pressure in the veins and a higher likelihood of clot formation.
- Smoking: Tobacco use damages blood vessels and alters blood flow, contributing to clot formation.
- Advanced Age: The risk of DVT and PE increases with age due to reduced mobility and changes in blood composition.
- Medical Conditions: Chronic heart failure, chronic obstructive pulmonary disease (COPD), and inflammatory bowel disease are among the conditions that elevate PE risk.
- Previous History of VTE: Individuals with a prior episode of deep vein thrombosis or pulmonary embolism have a higher risk of recurrence.
These risk factors interact with each other, so individuals with multiple risk factors have a significantly increased likelihood of developing a pulmonary embolism.
3. Symptoms
Symptoms of respiratory (pulmonary) embolism are often sudden in onset and can range from mild to life-threatening. The presentation is variable, and some patients may have minimal symptoms despite a significant embolic burden.
3.1 Common Symptoms
- Sudden Shortness of Breath (Dyspnea): This is the most common symptom of a pulmonary embolism, occurring even at rest in severe cases.
- Chest Pain: Often described as sharp, pleuritic chest pain that worsens with deep breaths, coughing, or movement.
- Rapid Heart Rate (Tachycardia): The heart may beat faster in an attempt to maintain adequate circulation.
- Cough: This may be dry or may produce blood-streaked sputum (hemoptysis).
- Anxiety or a Sense of Impending Doom: Many patients describe a feeling of intense anxiety or fear when experiencing a PE.
- Dizziness or Fainting (Syncope): Reduced oxygenation and low blood pressure can lead to fainting episodes.
- Cyanosis: A bluish tinge to the lips or skin may occur in severe cases due to low oxygen levels.
3.2 Additional Signs and Variability in Presentation
- Leg Symptoms: Some patients may also experience symptoms of deep vein thrombosis, such as pain, swelling, redness, or warmth in the leg.
- Hemodynamic Instability: In massive PE, signs of shock (e.g., low blood pressure, rapid, weak pulse) may be present.
- Right Ventricular Strain: Although not directly observable without imaging, symptoms such as fatigue and reduced exercise tolerance may be related to strain on the right ventricle.
- Asymptomatic Cases: In some instances, particularly with small emboli, patients may have minimal symptoms or be entirely asymptomatic, and the condition may be discovered incidentally during imaging for other reasons.
Because the symptoms of pulmonary embolism can mimic other conditions, a high index of suspicion is essential, especially in patients with known risk factors.
4. Diagnostic Exams and Tests
Accurate and timely diagnosis of pulmonary embolism is critical due to its potential severity. Diagnosis is based on a combination of clinical assessment, laboratory tests, imaging studies, and sometimes invasive hemodynamic monitoring.
4.1 Clinical Assessment
- Medical History and Physical Examination:
- A detailed history focusing on the onset and nature of symptoms (e.g., sudden shortness of breath, chest pain, cough) and risk factors (e.g., recent surgery, immobility, prior clots).
- Physical examination may reveal tachypnea, tachycardia, and signs of deep vein thrombosis (e.g., leg swelling, tenderness).
4.2 Laboratory Tests
- D-dimer Test:
- D-dimer is a fibrin degradation product. Elevated levels indicate active clot formation and breakdown, although it is non-specific.
- A normal D-dimer level can effectively rule out PE in patients with a low to intermediate pretest probability.
- Arterial Blood Gas (ABG):
- ABG may show hypoxemia (low oxygen levels), hypocapnia (low carbon dioxide levels) due to hyperventilation, and respiratory alkalosis.
- Cardiac Biomarkers:
- Elevated troponin levels and brain natriuretic peptide (BNP) may indicate right ventricular strain, especially in more severe PE.
4.3 Imaging Studies
4.3.1 Chest X-ray
- Utility:
- Although a chest X-ray is not diagnostic for PE, it helps rule out other causes of symptoms such as pneumonia, pneumothorax, or heart failure.
- It may be normal or show nonspecific findings such as atelectasis or pleural effusion.
4.3.2 Computed Tomographic Pulmonary Angiography (CTPA)
- Gold Standard Imaging:
- CTPA is the most widely used diagnostic test for pulmonary embolism.
- It provides detailed images of the pulmonary arteries, allowing for the identification of clots even in small branches.
- Contrast Use:
- Iodinated contrast is used to enhance visualization, though care must be taken in patients with renal insufficiency or contrast allergies.
4.3.3 Ventilation-Perfusion (V/Q) Scan
- Alternative Imaging:
- V/Q scanning is especially useful in patients for whom CTPA is contraindicated (e.g., pregnant women or those with contrast allergies).
- It assesses the matching of ventilation (air flow) and perfusion (blood flow) in the lungs. Mismatches can indicate a PE.
4.3.4 Echocardiography
- Assessment of Right Heart Function:
- While not diagnostic for PE, echocardiography can reveal signs of right ventricular strain, dilation, or dysfunction, which may support the diagnosis.
- It is particularly valuable in hemodynamically unstable patients.
4.3.5 Ultrasound of the Legs (Duplex Ultrasound)
- DVT Detection:
- Since most pulmonary embolisms originate from deep vein thrombosis in the legs, ultrasound is used to identify DVT.
- A positive ultrasound in a patient with suspected PE supports the diagnosis and guides treatment.
4.3.6 Pulmonary Angiography
- Invasive Gold Standard:
- Traditionally considered the definitive diagnostic test, pulmonary angiography is now reserved for cases where other imaging modalities are inconclusive or when interventional treatment is planned.
4.4 Clinical Prediction Rules
- Wells Score:
- A clinical prediction rule used to estimate the probability of pulmonary embolism based on patient history and clinical findings.
- Pulmonary Embolism Rule-out Criteria (PERC):
- A set of criteria used to identify patients at very low risk for PE who may not need further testing.
Using these tools alongside laboratory and imaging studies helps clinicians stratify risk and tailor diagnostic strategies.
5. Treatment Options
Treatment for pulmonary embolism focuses on preventing clot propagation, reducing the risk of further clot formation, and resolving the existing clot. The chosen therapy depends on the severity of the embolism, the patient’s clinical stability, and any contraindications to treatment.
5.1 Supportive and Initial Management
5.1.1 Immediate Care
- Oxygen Therapy:
- Administer supplemental oxygen to maintain adequate oxygen saturation.
- Stabilization:
- Monitor vital signs and initiate intravenous access.
- Provide analgesia for chest pain.
- Hemodynamic Support:
- In patients with hemodynamic instability (e.g., low blood pressure), supportive measures such as intravenous fluids, vasopressors, or inotropes may be necessary.
- Resuscitation:
- In cases of cardiac arrest suspected to be caused by massive PE, follow advanced life support protocols, including consideration of thrombolytic therapy.
5.2 Anticoagulation Therapy
Anticoagulants are the mainstay of treatment for pulmonary embolism, preventing further clot formation and allowing the body to gradually dissolve the existing clot.
5.2.1 Initial Anticoagulation
- Heparin:
- Unfractionated heparin (UFH) is often used in the hospital setting, particularly in unstable patients, due to its rapid onset and reversibility.
- Low molecular weight heparin (LMWH) is preferred for stable patients because of its predictable pharmacokinetics and ease of dosing.
- Fondaparinux:
- A synthetic factor Xa inhibitor that can be used as an alternative to LMWH.
5.2.2 Transition to Oral Anticoagulants
- Vitamin K Antagonists (VKAs):
- Warfarin has been the traditional choice. It requires bridging with heparin until therapeutic INR (usually between 2.0 and 3.0) is achieved.
- Direct Oral Anticoagulants (DOACs):
- Agents such as rivaroxaban, apixaban, dabigatran, and edoxaban offer fixed dosing and do not require routine INR monitoring.
- DOACs have become preferred in many cases due to ease of use and a lower risk of certain bleeding complications.
5.2.3 Duration of Anticoagulation
- Provoked PE:
- Typically treated for at least three months.
- Unprovoked PE or Persistent Risk Factors:
- May require extended or even lifelong anticoagulation.
- Recurrent VTE:
- Longer duration of therapy is usually warranted.
5.3 Thrombolytic Therapy
Thrombolysis, or clot-busting treatment, is indicated in patients with massive pulmonary embolism causing hemodynamic instability.
- Systemic Thrombolysis:
- Intravenous administration of thrombolytic agents (e.g., tissue plasminogen activator, tPA) can rapidly dissolve the clot.
- Thrombolysis is associated with a higher risk of bleeding, including intracranial hemorrhage, and is used when the benefits outweigh the risks.
- Catheter-Directed Thrombolysis (CDT):
- Involves the insertion of a catheter directly into the pulmonary artery to deliver thrombolytic agents locally.
- CDT is often used in patients who have contraindications to systemic thrombolysis or when a targeted approach is desired.
5.4 Mechanical and Surgical Interventions
In cases where thrombolysis is contraindicated or ineffective, or if the patient is hemodynamically unstable, more invasive procedures may be considered.
5.4.1 Catheter-Directed Thrombectomy
- Procedure:
- A catheter is inserted into the pulmonary artery to physically remove or fragment the clot.
- Often combined with local thrombolysis.
- Benefits:
- Provides rapid improvement in hemodynamics with a lower risk of bleeding compared to systemic thrombolysis.
5.4.2 Surgical Pulmonary Embolectomy
- Indications:
- Reserved for patients with massive PE who are not candidates for thrombolysis or catheter-directed interventions.
- Risks:
- Invasive procedure with associated surgical risks; usually considered as a last resort.
5.4.3 Inferior Vena Cava (IVC) Filters
- Use:
- Indicated in patients who cannot receive anticoagulation or who develop recurrent clots despite adequate anticoagulation.
- Temporary vs. Permanent:
- Retrievable filters are preferred; they should be removed as soon as it is safe to resume anticoagulation.
- Limitations:
- Filters do not treat the existing embolism and carry their own risks, including filter thrombosis and migration.
5.5 Long-Term Management and Follow-Up
Following acute treatment, long-term management is focused on preventing recurrence and managing any chronic complications.
- Ongoing Anticoagulation:
- Continuation of blood-thinning medication as prescribed, with regular monitoring (e.g., INR for warfarin).
- Rehabilitation:
- Gradual return to physical activity and exercise programs tailored to improve cardiovascular fitness.
- Monitoring for Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
- In some patients, repeated episodes of PE can lead to CTEPH, which requires ongoing evaluation and management.
- Patient Education:
- Empower patients with knowledge about symptoms of recurrent VTE, medication adherence, and lifestyle modifications.
6. Available Support Groups and Resources
Dealing with pulmonary embolism can be challenging, both physically and emotionally. Various support groups and resources are available to help patients and their families cope with the condition.
6.1 National and International Organizations
- Pulmonary Embolism Response Team (PERT) Networks:
- Multidisciplinary teams that not only manage acute PE but also provide patient education and support.
- American Heart Association (AHA):
- Provides comprehensive information on heart and vascular diseases, including pulmonary embolism, along with patient support initiatives.
- National Blood Clot Alliance:
- A resource dedicated to raising awareness about blood clots and providing support to survivors of VTE.
- Venous Thromboembolism (VTE) Foundation:
- Offers educational materials and support networks for individuals with DVT and PE.
- European Society of Cardiology (ESC):
- Provides guidelines and patient education resources for cardiovascular conditions, including PE.
- Mayo Clinic and Cleveland Clinic Patient Resources:
- Both institutions offer patient education, support group information, and guidance for managing PE.
6.2 Online Communities and Forums
- HealthUnlocked, Inspire, and Reddit:
- Online platforms where patients share experiences, treatment tips, and support.
- Facebook Groups:
- Numerous groups are dedicated to VTE and PE, where patients and caregivers discuss management strategies and personal experiences.
6.3 Local Support Groups
- Hospital-Based Support Groups:
- Many hospitals have support groups for patients with thromboembolic diseases, providing face-to-face interaction and shared experiences.
- Community Health Organizations:
- Local organizations and clinics may offer meetings, educational sessions, and counseling services tailored to patients with PE.
6.4 Educational Materials and Resources
- Patient Brochures and Guides:
- Materials provided by organizations like the AHA, NHLBI, and National Blood Clot Alliance.
- Webinars and Workshops:
- Many organizations host online and in-person events focusing on blood clot prevention, treatment updates, and coping strategies.
- Patient Navigation Programs:
- Programs that help patients coordinate care, understand their treatment plan, and access available resources.
7. Prognosis and Long-Term Outlook
7.1 Prognosis Overview
The prognosis for pulmonary embolism varies widely depending on several factors:
- Severity of the Embolism:
- Massive PE, characterized by hemodynamic instability, carries a higher mortality rate.
- Small or subsegmental PEs generally have a better prognosis.
- Timeliness of Diagnosis and Treatment:
- Early intervention can significantly reduce the risk of mortality and long-term complications.
- Patient’s Overall Health:
- Underlying conditions such as cancer, heart disease, or chronic lung disease can worsen the prognosis.
- Risk of Recurrence:
- Patients with unprovoked PE or persistent risk factors have a higher likelihood of recurrent events.
7.2 Long-Term Outcomes
- Mortality:
- With prompt treatment, mortality rates for PE have decreased, though PE remains a significant cause of cardiovascular death.
- Chronic Complications:
- Some patients develop chronic thromboembolic pulmonary hypertension (CTEPH), a condition in which repeated embolic events lead to long-term increases in pulmonary arterial pressure.
- Quality of Life:
- Many survivors experience improvements in symptoms with appropriate treatment, but some may have lingering issues such as reduced exercise capacity or persistent right heart dysfunction.
- Recurrence:
- The risk of recurrence depends on the duration of anticoagulation and the presence of reversible versus persistent risk factors.
7.3 Prognostic Tools
- Pulmonary Embolism Severity Index (PESI) and Simplified PESI (sPESI):
- These scoring systems help predict 30-day mortality in patients with acute PE and guide treatment decisions.
- Right Ventricular Function:
- Echocardiographic assessment of right ventricular function is a key prognostic indicator.
Patients with lower risk scores and preserved right ventricular function generally have a more favorable prognosis.
8. Possible Complications
Pulmonary embolism can lead to several acute and chronic complications:
8.1 Acute Complications
- Hemodynamic Instability and Shock:
- Massive PE can cause a significant drop in blood pressure, leading to obstructive shock and, in severe cases, cardiac arrest.
- Right Heart Failure:
- Increased resistance in the pulmonary arteries places strain on the right ventricle, which may eventually fail.
- Pulmonary Infarction:
- When the blood supply to a portion of the lung is completely blocked, lung tissue may die (infarct), leading to pleuritic pain and sometimes hemoptysis.
- Arrhythmias:
- Heart rhythm abnormalities, including atrial fibrillation, may develop due to right ventricular strain.
- Hypoxemia:
- Inadequate oxygenation of the blood can occur, leading to cyanosis and multi-organ dysfunction.
8.2 Chronic Complications
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
- Persistent or recurrent clots can lead to chronic pulmonary hypertension, significantly affecting quality of life and survival.
- Recurrent Venous Thromboembolism (VTE):
- Without adequate anticoagulation or in the presence of persistent risk factors, patients may experience recurrent episodes of DVT or PE.
- Post-Thrombotic Syndrome:
- Following DVT, some patients may develop chronic leg pain, swelling, and skin changes due to venous damage.
Long-term management and regular follow-up are essential to minimize these complications.
9. Indications for Seeking Medical Attention
Prompt recognition and treatment of pulmonary embolism are critical. Seek immediate medical attention if you experience:
- Sudden Onset Shortness of Breath:
- Especially if it occurs at rest or is accompanied by chest pain.
- Chest Pain:
- Sharp, pleuritic chest pain that worsens with deep breaths.
- Cough:
- Particularly if it includes blood or blood-tinged sputum.
- Rapid Heart Rate or Palpitations:
- New or worsening tachycardia.
- Dizziness or Fainting (Syncope):
- Indicating reduced blood flow to the brain.
- Swelling or Pain in the Legs:
- Signs of deep vein thrombosis (DVT) that might indicate a clot in the leg.
- Signs of Hemodynamic Instability:
- Low blood pressure, severe fatigue, or altered mental status.
If you or someone you are with experiences these symptoms, especially if risk factors for PE are present, seek emergency care immediately.
10. Preventive Measures and Self-Care Strategies
Preventing pulmonary embolism primarily focuses on reducing the risk of deep vein thrombosis (DVT), as DVT is the most common precursor to PE. Strategies include:
10.1 Lifestyle Modifications
10.1.1 Regular Physical Activity
- Exercise:
- Engage in regular, moderate physical activity to improve blood circulation and reduce the risk of clot formation.
- Movement:
- Avoid prolonged periods of inactivity, especially during long-haul flights or after surgery. Even simple leg exercises can promote blood flow.
10.1.2 Healthy Diet and Weight Management
- Diet:
- A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports overall health and reduces obesity—a risk factor for clot formation.
- Hydration:
- Drinking plenty of water helps maintain proper blood viscosity and circulation.
10.1.3 Avoid Smoking
- Smoking Cessation:
- Smoking damages blood vessels and increases clotting risk. Quitting smoking is one of the most effective preventive measures.
10.2 Preventive Therapies
10.2.1 Pharmacologic Prophylaxis
- Anticoagulants:
- For individuals at high risk (e.g., post-surgery, prolonged immobility, cancer patients), prophylactic anticoagulation with low molecular weight heparin or other agents may be recommended.
- Aspirin:
- In some cases, low-dose aspirin is used as a preventive measure against clot formation.
10.2.2 Mechanical Prophylaxis
- Compression Stockings:
- Graduated compression stockings help improve venous return from the legs.
- Pneumatic Compression Devices:
- Devices that intermittently compress the legs can be used in hospitalized patients to prevent DVT.
10.3 Special Considerations
- Pregnancy:
- Pregnant women, particularly those with additional risk factors, should discuss prophylactic measures with their healthcare provider. Anticoagulant therapy (usually LMWH) is often used safely during pregnancy.
- Postoperative Care:
- After surgery, particularly orthopedic procedures, early mobilization and prophylactic anticoagulation are critical.
- Long-Haul Travel:
- For individuals at risk, moving around and wearing compression stockings during long journeys can help prevent DVT.
10.4 Patient Education
- Symptom Awareness:
- Educate yourself on the symptoms of DVT and PE. Early recognition of signs such as leg swelling, pain, and shortness of breath can be life-saving.
- Adherence to Treatment:
- If prescribed anticoagulants or other medications, take them exactly as directed.
- Communication with Healthcare Providers:
- Discuss any concerns, risk factors, or family history of blood clots with your doctor.
By incorporating these preventive measures, you can significantly reduce your risk of developing a pulmonary embolism.
11. References and Credible Medical Sources
The information in this guide is based on current clinical guidelines, peer-reviewed literature, and reputable medical resources. Key references include:
Mayo Clinic: “Pulmonary Embolism – Symptoms and Causes.”
https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647American Heart Association (AHA): Information on pulmonary embolism, diagnosis, and treatment.
https://www.heart.org/en/health-topics/pulmonary-embolismNational Heart, Lung, and Blood Institute (NHLBI): “What Is Pulmonary Embolism?”
https://www.nhlbi.nih.gov/health-topics/pulmonary-embolismMedlinePlus (U.S. National Library of Medicine): “Pulmonary Embolism.”
https://medlineplus.gov/pulmonaryembolism.htmlJohns Hopkins Medicine: “Pulmonary Embolism.”
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pulmonary-embolismMerck Manuals: “Pulmonary Embolism (PE).”
https://www.merckmanuals.com/professional/pulmonary-disorders/pulmonary-embolism/pulmonary-embolism-peStatPearls: “Acute Pulmonary Embolism.”
https://www.ncbi.nlm.nih.gov/books/NBK560551/European Society of Cardiology (ESC) Guidelines:
Galiè N, et al. “2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism.” Eur Heart J. 2019.UpToDate: “Evaluation and Management of Pulmonary Embolism.” (Subscription required)
National Blood Clot Alliance: Educational resources on pulmonary embolism and deep vein thrombosis.
World Health Organization (WHO): Information on global health and venous thromboembolism.
Cleveland Clinic: “Pulmonary Embolism.”
https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism