Pulmonary hypertension (PH) is a serious and progressive condition characterized by high blood pressure in the pulmonary arteries, which carry blood from the heart to the lungs. Unlike systemic hypertension, which affects the entire body, pulmonary hypertension specifically impacts the blood vessels in the lungs, ultimately placing strain on the right side of the heart. This guide provides an extensive overview of pulmonary hypertension—including its definition, alternative names, causes, common symptoms, diagnostic tests, treatment options, support resources, prognosis, possible complications, indications for seeking medical care, and preventive measures.
1. Definition and Alternative Names
1.1 What Is Pulmonary Hypertension?
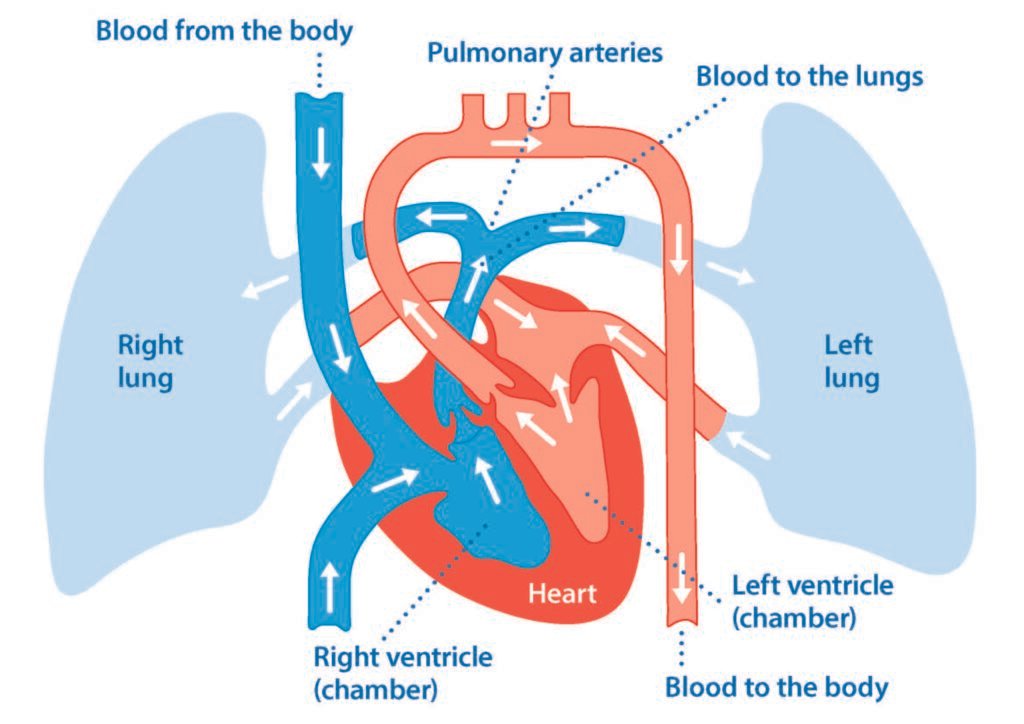
Pulmonary hypertension is defined as a mean pulmonary arterial pressure (mPAP) of 25 mm Hg or higher at rest, as measured by right heart catheterization. In PH, the small arteries in the lungs become narrowed, blocked, or destroyed, which increases the resistance to blood flow. As the right ventricle of the heart works harder to pump blood through these constricted vessels, it may eventually lead to right heart failure. PH is not a single disease but rather a spectrum of conditions with various underlying causes.
1.2 Alternative Names
Depending on its cause and presentation, pulmonary hypertension may be referred to by several names:
- Pulmonary Arterial Hypertension (PAH): A specific subset of PH (World Health Organization Group 1) characterized by vascular remodeling in the pulmonary arteries.
- Pulmonary Vascular Disease: A broader term that includes all disorders affecting the pulmonary blood vessels.
- Primary Pulmonary Hypertension: An older term often used interchangeably with idiopathic pulmonary arterial hypertension (IPAH), although it is now less favored.
- Secondary Pulmonary Hypertension: Used when PH is caused by other underlying conditions (e.g., left heart disease, lung diseases, chronic thromboembolic PH).
Understanding these terms is essential because the underlying cause of PH guides treatment decisions and prognosis.
2. Causes and Risk Factors
Pulmonary hypertension is a multifactorial condition with diverse etiologies. The causes and risk factors vary depending on the type of PH, which is classified into five groups by the World Health Organization (WHO).
2.1 WHO Classification of Pulmonary Hypertension
- Group 1 – Pulmonary Arterial Hypertension (PAH):
- Idiopathic (IPAH)
- Heritable (due to genetic mutations, such as BMPR2)
- Associated with connective tissue diseases (e.g., scleroderma, lupus)
- Congenital heart disease (repaired or unrepaired)
- Drugs and toxins (e.g., appetite suppressants)
- Group 2 – PH Due to Left Heart Disease:
- Left ventricular systolic or diastolic dysfunction
- Valvular heart disease (e.g., mitral or aortic stenosis/regurgitation)
- Group 3 – PH Due to Lung Diseases and/or Hypoxia:
- Chronic obstructive pulmonary disease (COPD)
- Interstitial lung disease
- Sleep-disordered breathing (obstructive sleep apnea)
- Chronic exposure to high altitude
- Group 4 – Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
- Persistent blood clots in the pulmonary arteries
- Group 5 – PH with Unclear or Multifactorial Mechanisms:
- Hematologic disorders, metabolic disorders, or other conditions
2.2 Causes
Each group has distinct causes:
- Idiopathic PAH: No identifiable cause but may be linked to genetic predisposition (e.g., BMPR2 mutations).
- Heritable PAH: Inherited genetic mutations increase the risk.
- Connective Tissue Diseases: Inflammatory processes in diseases like scleroderma can cause pulmonary vascular remodeling.
- Left Heart Disease: Conditions such as heart failure or valvular disorders can lead to a backup of pressure into the pulmonary circulation.
- Lung Diseases: Chronic lung conditions or hypoxia from sleep apnea can trigger vasoconstriction in the pulmonary arteries.
- Chronic Thromboembolism: Recurrent or unresolved pulmonary emboli can lead to persistent blockage of pulmonary vessels.
- Drugs and Toxins: Certain medications (e.g., methamphetamine, appetite suppressants) and toxins have been linked to PH.
2.3 Risk Factors
- Genetic Predisposition: Family history of PAH or heritable mutations.
- Underlying Diseases: Presence of connective tissue disorders, left heart disease, or chronic lung disease.
- Lifestyle Factors: Smoking, sedentary lifestyle, and exposure to high altitudes.
- Medications: Long-term use of certain drugs may predispose individuals.
- Age and Gender: PAH is more common in young to middle-aged women, though PH due to left heart disease or lung disease typically affects older individuals.
3. Symptoms of Pulmonary Hypertension
The symptoms of pulmonary hypertension often develop gradually and can be nonspecific, which makes early diagnosis challenging. They primarily result from the heart’s struggle to overcome increased resistance in the pulmonary vasculature.
3.1 Common Symptoms
- Shortness of Breath (Dyspnea): Initially occurs with exertion but may progress to dyspnea at rest as the disease worsens.
- Fatigue: Persistent tiredness and reduced exercise tolerance are common.
- Chest Pain (Angina): Due to the increased workload on the right ventricle and reduced oxygen delivery.
- Palpitations: Awareness of an irregular or fast heartbeat.
- Syncope (Fainting): Sudden loss of consciousness, especially during exertion, due to decreased cardiac output.
- Edema: Swelling in the ankles, legs, and sometimes abdomen (ascites), typically due to right heart failure.
- Cyanosis: A bluish tint to the lips and skin may occur in advanced stages, indicating severe oxygen deprivation.
3.2 Additional and Nonspecific Symptoms
- Dizziness and Lightheadedness: Often related to low oxygen levels and decreased cardiac output.
- Reduced Exercise Capacity: Patients may notice a significant decrease in their ability to perform physical activities.
- Weakness: Generalized weakness and a feeling of being unwell.
- Cough: Often a dry cough, which may be persistent.
- Respiratory Infections: Recurrent respiratory infections due to reduced lung perfusion.
- Abdominal Discomfort: In advanced cases, congestion of the liver and abdomen can cause discomfort or pain.
3.3 Symptom Progression
Early in the disease, symptoms may be mild and easily attributed to other causes, such as lack of fitness. As pulmonary hypertension advances, however, the increased strain on the right side of the heart and the reduced oxygenation of body tissues lead to more pronounced and disabling symptoms. This gradual progression often results in delayed diagnosis.
4. Diagnostic Exams and Tests
Early detection of pulmonary hypertension is essential for optimal management. A combination of clinical evaluation, imaging studies, and specialized tests is used to diagnose PH and determine its severity.
4.1 Clinical Evaluation
- Medical History: A thorough history includes assessment of symptoms (e.g., shortness of breath, fatigue, chest pain), family history of pulmonary hypertension or heart disease, and evaluation of risk factors such as connective tissue disorders or left heart disease.
- Physical Examination: A detailed exam may reveal signs such as a loud second heart sound (accentuated P2), murmurs, jugular venous distension, peripheral edema, and signs of right heart failure.
4.2 Laboratory Tests
- Blood Tests: Blood tests assess for anemia, thyroid function, liver and kidney function, and biomarkers such as brain natriuretic peptide (BNP) or NT-proBNP, which are elevated in heart failure and can indicate the severity of PH.
- Autoimmune Screening: Tests for connective tissue diseases (e.g., ANA, rheumatoid factor) may be performed if a connective tissue disorder is suspected.
4.3 Imaging Studies
- Chest X-ray: Provides a preliminary view of the heart and lungs. It may show an enlarged right ventricle, pulmonary artery dilation, or signs of lung disease.
- Echocardiography: A noninvasive ultrasound of the heart is the primary screening tool for PH. It estimates pulmonary arterial pressure, evaluates right ventricular size and function, and assesses for other cardiac abnormalities.
- Cardiac MRI: Offers detailed images of cardiac structure and function, especially useful when echocardiography results are inconclusive.
- Ventilation-Perfusion (V/Q) Scan: Particularly useful in evaluating chronic thromboembolic pulmonary hypertension (CTEPH) by assessing the distribution of blood flow in the lungs.
- CT Pulmonary Angiography: Used to visualize the pulmonary arteries and detect chronic or acute emboli that could contribute to PH.
4.4 Hemodynamic Assessment
- Right Heart Catheterization: The gold standard for diagnosing pulmonary hypertension. This invasive procedure directly measures the pulmonary arterial pressure, pulmonary capillary wedge pressure, and cardiac output. It confirms the diagnosis and helps determine the severity and type of PH.
4.5 Additional Tests
- Six-Minute Walk Test: Assesses exercise capacity and oxygen saturation during physical exertion. It provides a functional measure of disease severity and response to therapy.
- Pulmonary Function Tests (PFTs): Evaluate lung volumes and gas exchange, especially when lung disease is suspected as the underlying cause.
- Electrocardiogram (ECG): May show signs of right ventricular hypertrophy or strain.
- Blood Oxygen Saturation Monitoring: Pulse oximetry and arterial blood gas analysis help assess the degree of hypoxemia.
5. Treatment Options
Management of pulmonary hypertension is complex and requires a multidisciplinary approach tailored to the underlying cause and the severity of the disease. Treatment options include lifestyle modifications, medications, and in some cases, surgical interventions.
5.1 Lifestyle and Supportive Measures
5.1.1 Lifestyle Modifications
- Exercise: Regular, moderate exercise (as tolerated) can improve functional capacity and overall well-being. Exercise regimens should be individualized and supervised by healthcare professionals.
- Diet: A heart-healthy diet that is low in sodium, saturated fats, and cholesterol can help manage fluid retention and reduce strain on the heart.
- Weight Management: Maintaining a healthy weight is important to reduce the overall workload on the cardiovascular system.
- Avoiding High Altitude: Exposure to high altitude may worsen symptoms due to lower oxygen levels.
5.1.2 Supportive Care
- Oxygen Therapy: Supplemental oxygen may be required, especially in patients with low blood oxygen levels or those experiencing severe hypoxemia.
- Diuretics: Medications such as furosemide help manage fluid retention by reducing the volume of circulating blood and alleviating symptoms of right heart failure.
- Anticoagulants: In cases where there is a risk of thromboembolism (especially in chronic thromboembolic PH), blood thinners may be used to prevent blood clots.
- Vaccinations: Keeping up-to-date with influenza, pneumococcal, and other vaccines is important to prevent respiratory infections that can exacerbate PH.
5.2 Disease-Specific Medications
The treatment of pulmonary hypertension often involves several classes of medications aimed at reducing pulmonary arterial pressure, improving symptoms, and enhancing quality of life.
5.2.1 Endothelin Receptor Antagonists (ERAs)
- Examples: Bosentan, Ambrisentan, Macitentan.
- Mechanism: These drugs block the action of endothelin-1, a potent vasoconstrictor, thereby helping to relax the pulmonary arteries and lower blood pressure.
- Benefits: They have been shown to improve exercise capacity and delay disease progression.
5.2.2 Phosphodiesterase-5 (PDE5) Inhibitors
- Examples: Sildenafil, Tadalafil.
- Mechanism: PDE5 inhibitors promote vasodilation by increasing levels of cyclic guanosine monophosphate (cGMP) in the pulmonary vasculature.
- Benefits: They can improve exercise capacity, reduce symptoms, and enhance quality of life.
5.2.3 Prostacyclin Analogues and Receptor Agonists
- Examples: Epoprostenol, Iloprost, Treprostinil, Selexipag.
- Mechanism: These medications mimic the effects of prostacyclin, a natural vasodilator that also inhibits platelet aggregation.
- Benefits: They are effective in reducing pulmonary arterial pressure and are particularly useful in severe cases of PAH. Epoprostenol, for example, is administered intravenously and has a rapid onset of action.
5.2.4 Soluble Guanylate Cyclase (sGC) Stimulators
- Example: Riociguat.
- Mechanism: sGC stimulators enhance the nitric oxide (NO) pathway, leading to vasodilation of the pulmonary arteries.
- Benefits: Particularly useful in patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are not candidates for surgery.
5.2.5 Calcium Channel Blockers
- Usage: Calcium channel blockers may be used in a small subset of patients who demonstrate a positive acute vasoreactivity test during right heart catheterization.
- Caution: Only a minority of patients respond to these medications, and they are not used routinely.
5.3 Advanced and Interventional Treatments
For patients with severe pulmonary hypertension who do not respond to medical therapy, advanced treatments may be considered.
5.3.1 Atrial Septostomy
- Procedure: A procedure that creates a small hole between the right and left atria of the heart to decompress the right side. It can temporarily improve symptoms and quality of life in select patients.
- Indications: Typically reserved for patients with severe, refractory PH.
5.3.2 Lung Transplantation
- Procedure: Lung or heart–lung transplantation is considered in patients with end-stage pulmonary hypertension.
- Considerations: Due to the complexity and risks of transplantation, this option is reserved for patients who have exhausted other therapies.
- Prognosis: Transplantation can significantly improve survival and quality of life but carries its own risks of rejection and complications.
5.3.3 Balloon Pulmonary Angioplasty (BPA)
- Usage: Primarily used in patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are not surgical candidates.
- Procedure: BPA involves dilating the narrowed pulmonary arteries using a balloon catheter, improving blood flow and reducing pulmonary pressures.
5.4 Combination Therapy
In many cases, a combination of medications is used to target different pathways involved in PH. For example, a patient might be treated with an endothelin receptor antagonist along with a PDE5 inhibitor. Combination therapy may offer a synergistic effect, improving overall outcomes and delaying disease progression.
6. Available Support Groups and Resources
Living with pulmonary hypertension can be challenging, and support is crucial to help patients manage the emotional and psychological aspects of the disease. There are many resources available, including national organizations, online communities, and local support groups.
6.1 National and International Organizations
- Pulmonary Hypertension Association (PHA): Offers educational materials, patient support programs, advocacy, and local chapters for in-person support.
- American Heart Association (AHA): Provides information on heart and lung diseases, including pulmonary hypertension, along with community support and research updates.
- National Heart, Lung, and Blood Institute (NHLBI): Offers comprehensive information about PH, current research, clinical trials, and treatment guidelines.
- European Society of Cardiology (ESC): Provides resources and guidelines for European patients with pulmonary hypertension.
- World Health Organization (WHO): Offers global data and strategies for managing chronic conditions such as PH.
6.2 Online Communities and Forums
- HealthUnlocked: A social network where patients with pulmonary hypertension share experiences and support each other.
- Inspire: An online community for patients with various conditions, including PH.
- Reddit: Subreddits like r/PulmonaryHypertension allow patients and caregivers to exchange advice and personal stories.
- Facebook Groups: Many groups focus on pulmonary hypertension support, offering updates on research and treatment experiences.
6.3 Local and Regional Support Groups
Many hospitals and clinics have specialized pulmonary hypertension clinics that offer support groups and educational sessions. Ask your healthcare provider for local resources, which may include:
- Pulmonary Hypertension Clinics: These multidisciplinary clinics provide comprehensive care, including access to social workers and mental health professionals.
- Patient Advocacy Groups: Local chapters of national organizations like the Pulmonary Hypertension Association often hold meetings and events for patient support.
6.4 Educational Materials
- Books and Brochures: Numerous publications provide detailed information on PH, management strategies, and patient experiences.
- Webinars and Workshops: Many organizations offer online seminars and local workshops to educate patients and caregivers about living with pulmonary hypertension.
- Patient Navigation Programs: Some centers offer patient navigators to help individuals understand their condition, access resources, and coordinate care.
7. Prognosis and Long-Term Outlook
7.1 Prognosis Overview
Pulmonary hypertension is a chronic and progressive condition. Prognosis varies widely depending on the underlying cause, severity of the disease, and the patient’s response to treatment. Although advances in treatment have improved outcomes, PH remains a serious condition that can reduce life expectancy and quality of life.
- Pulmonary Arterial Hypertension (Group 1): Patients with idiopathic or heritable PAH historically had a poor prognosis, with median survival of 2–3 years if untreated. However, with modern therapies, survival has improved significantly.
- PH Due to Left Heart Disease or Lung Disease (Groups 2 and 3): Prognosis is closely tied to the severity of the underlying cardiac or pulmonary condition.
- Chronic Thromboembolic PH (Group 4): Patients may have a better outlook if they are candidates for surgical treatment (pulmonary thromboendarterectomy) or balloon pulmonary angioplasty.
- Overall Impact: With current therapies and comprehensive care, many patients experience symptom relief and improved quality of life. Nonetheless, the progressive nature of PH means that patients require long-term follow-up and management.
7.2 Factors Influencing Prognosis
Several factors are associated with a poorer prognosis in PH:
- Severity of Symptoms: Advanced functional class (III–IV) on the World Health Organization (WHO) scale is associated with worse outcomes.
- Right Heart Function: Poor right ventricular function, as assessed by echocardiography or cardiac MRI, correlates with reduced survival.
- Biomarkers: Elevated levels of NT-proBNP (N-terminal pro-brain natriuretic peptide) and troponin are linked to adverse outcomes.
- Response to Therapy: Patients who show minimal improvement with standard treatments may have a more aggressive disease course.
- Underlying Cause: Prognosis is generally worse for patients with idiopathic PAH or PAH associated with connective tissue diseases than for those with PH secondary to left heart or lung diseases.
7.3 Long-Term Outlook
- Improved Survival: With modern therapies, patients with PAH now have a significantly longer life expectancy than in previous decades.
- Quality of Life: Ongoing management can help improve exercise capacity and overall quality of life, although patients may still experience limitations and require supportive care.
- Ongoing Monitoring: Regular assessments and adjustments in treatment are critical to maintaining stability and delaying disease progression.
8. Possible Complications
Pulmonary hypertension can lead to several complications, particularly if left untreated or if the disease progresses despite therapy.
8.1 Right Heart Failure
As the right ventricle struggles to pump blood against the high resistance in the pulmonary arteries, it may eventually fail:
- Symptoms: Peripheral edema, ascites, jugular venous distension, fatigue, and liver congestion.
- Management: Requires careful management with diuretics, oxygen, and advanced therapies.
8.2 Arrhythmias
Abnormal heart rhythms, including atrial fibrillation and ventricular arrhythmias, can develop due to the strain on the heart:
- Symptoms: Palpitations, dizziness, and syncope.
- Management: May require medications, cardioversion, or implantable devices.
8.3 Thromboembolic Events
Patients with PH, especially those with CTEPH, are at increased risk of blood clots:
- Pulmonary Embolism: Clots can further obstruct pulmonary blood flow.
- Deep Vein Thrombosis: In some cases, clots from the legs may travel to the lungs.
8.4 Hemoptysis
Coughing up blood may occur due to rupture of fragile, dilated vessels in the pulmonary circulation:
- Severity: Can range from mild to life-threatening.
- Management: Requires prompt evaluation and treatment.
8.5 Syncope
Fainting spells may occur, particularly during exertion, due to a transient drop in cardiac output:
- Implications: Syncope is a warning sign and may require adjustment in therapy.
- Management: Identifying and treating the underlying cause is crucial.
8.6 Multiorgan Dysfunction
Advanced pulmonary hypertension can eventually lead to dysfunction of other organs, particularly if right heart failure is present:
- Liver Congestion: Can lead to abnormal liver function tests and cirrhosis.
- Renal Impairment: Reduced cardiac output can impair kidney function.
9. Indications for Seeking Medical Attention
Early recognition and prompt treatment of pulmonary hypertension and its complications are critical. Patients and caregivers should be aware of signs that warrant immediate medical evaluation:
9.1 Worsening Shortness of Breath
- Exertional Dyspnea: Increasing difficulty breathing during routine activities may indicate disease progression.
- Resting Dyspnea: Shortness of breath at rest is a red flag and should prompt immediate evaluation.
9.2 Chest Pain
- Angina-Like Pain: Persistent or worsening chest pain, especially if it occurs with exertion, may indicate increased strain on the heart.
- Action: Seek prompt medical assessment.
9.3 Syncope or Dizziness
- Episodes of Fainting: Recurrent syncope or dizziness could signal a drop in cardiac output or arrhythmia.
- Action: Urgent evaluation is necessary.
9.4 Swelling in the Legs or Abdomen
- Edema: New or worsening swelling in the legs, ankles, or abdomen may indicate right heart failure.
- Action: Medical consultation is essential.
9.5 Rapid Heart Rate or Palpitations
- Irregular Heartbeat: If you experience a fast or irregular heartbeat, it could be a sign of arrhythmia.
- Action: Prompt evaluation can prevent further complications.
9.6 Worsening Fatigue or Reduced Exercise Capacity
- Functional Decline: Significant reductions in the ability to perform daily activities or exercise intolerance should be evaluated.
- Action: Discuss these changes with your healthcare provider.
9.7 Signs of Infection
- Fever, Cough, or Sputum Production: Given the risk of respiratory infections exacerbating PH, any signs of infection warrant prompt attention.
- Action: Seek care early to prevent complications such as acute respiratory failure.
10. Preventive Measures and Self-Care Strategies
Although pulmonary hypertension cannot be entirely prevented—especially when it is secondary to genetic or structural heart diseases—several measures can help manage the condition and reduce the risk of complications.
10.1 Lifestyle Modifications
10.1.1 Exercise and Physical Activity
- Regular, Moderate Exercise: Engage in regular physical activity as tolerated. Low-impact exercises such as walking, swimming, or cycling can improve cardiovascular fitness without overstraining the heart.
- Tailored Exercise Programs: Work with a cardiac rehabilitation specialist or physiotherapist to design an exercise plan that suits your condition.
10.1.2 Diet and Nutrition
- Heart-Healthy Diet: Focus on a diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats. Limit sodium intake to help manage fluid retention.
- Weight Management: Maintaining a healthy weight reduces the overall workload on the heart and improves overall health.
- Limit Alcohol and Caffeine: Both can affect blood pressure and hydration, so moderation is key.
10.1.3 Hydration
- Adequate Fluid Intake: Staying well-hydrated supports optimal blood flow and helps prevent thickening of the blood, which can worsen PH symptoms.
- Monitor Fluid Balance: In patients with right heart failure, fluid intake may need to be carefully monitored under medical guidance.
10.2 Medications and Adherence
- Strict Adherence: Taking medications as prescribed (e.g., ERAs, PDE5 inhibitors, prostacyclin analogues) is crucial for managing pulmonary pressures and improving symptoms.
- Regular Follow-Up: Ensure you attend all scheduled appointments for monitoring, including echocardiograms and lab tests.
10.3 Avoiding Triggers
- Avoid High Altitudes: High altitude can worsen hypoxemia. If travel is necessary, discuss precautions with your healthcare provider.
- Minimize Exposure to Infections: Practice good hygiene, avoid large crowds during flu season, and get vaccinated.
- Stress Management: Use relaxation techniques, counseling, and stress-reducing activities to manage emotional stress, which can impact heart rate and blood pressure.
10.4 Regular Screening and Monitoring
- Echocardiography: Regular heart ultrasounds to monitor right ventricular function and pulmonary artery pressures.
- Blood Tests: Periodic measurement of biomarkers like BNP or NT-proBNP, which can indicate heart strain.
- Functional Tests: Six-minute walk tests and exercise stress tests help gauge your functional capacity and guide treatment adjustments.
10.5 Patient Education
- Learn About Your Condition: Understanding pulmonary hypertension empowers you to recognize symptoms, adhere to treatment plans, and make informed decisions.
- Supportive Resources: Utilize online resources, brochures, and workshops provided by organizations such as the Pulmonary Hypertension Association.
- Family Involvement: Educate family members about PH so they can support you in managing the condition and recognizing when to seek help.
10.6 Preventive Care
- Vaccinations: Stay current with vaccinations, including influenza, pneumococcal, and COVID-19 vaccines, to prevent infections that can worsen PH.
- Regular Dental Care: Good oral hygiene can reduce the risk of infections that may trigger systemic inflammation.
- Avoid Smoking: Smoking is a major risk factor for worsening PH and should be avoided at all costs.
11. References and Credible Medical Sources
The information provided in this article is supported by a range of high-quality, peer-reviewed sources and reputable medical organizations. Key references include:
Mayo Clinic: “Pulmonary Hypertension.”
https://www.mayoclinic.org/diseases-conditions/pulmonary-hypertension/symptoms-causes/syc-20351413American Heart Association (AHA): Information on pulmonary hypertension, its symptoms, and treatment options.
https://www.heart.org/en/health-topics/pulmonary-hypertensionNational Heart, Lung, and Blood Institute (NHLBI): “What Is Pulmonary Hypertension?”
https://www.nhlbi.nih.gov/health-topics/pulmonary-hypertensionMedlinePlus (U.S. National Library of Medicine): “Pulmonary Hypertension.”
https://medlineplus.gov/pulmonaryhypertension.htmlJohns Hopkins Medicine: “Pulmonary Hypertension.”
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pulmonary-hypertensionPulmonary Hypertension Association (PHA): Comprehensive patient education and support resources for PH.
https://phassociation.org/UpToDate: Evidence-based clinical recommendations for pulmonary hypertension management (subscription required).
Peer-Reviewed Journals:
- Simonneau G, et al. “Updated clinical classification of pulmonary hypertension.” J Am Coll Cardiol. 2013;62(25 Suppl):D34-D41.
- Galiè N, et al. “2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension.” Eur Heart J. 2016;37(1):67-119.
Centers for Disease Control and Prevention (CDC): Information and statistics on pulmonary hypertension.
https://www.cdc.gov/pulmonaryhypertension/