What is juvenile idiopathic arthritis?
Juvenile idiopathic arthritis (JIA) is a form of arthritis in children. Arthritis causes joint swelling (inflammation) and joint stiffness. JIA is arthritis that affects 1 or more joints for at least 6 weeks in a child age 16 or younger.
Unlike adult rheumatoid arthritis, which is ongoing (chronic) and lasts a lifetime, children often outgrow JIA. But the disease can affect bone development in a growing child.
Affected Areas
Primarily, JIA affects joints like knees and wrists, but it can also involve eyes (causing uveitis) and, in systemic cases, organs like the heart and lungs.
Prevalence and Importance
It affects about 50,000 children in the US, with an incidence of 4-14 per 100,000 annually. Early management is crucial to prevent long-term joint damage and other health issues.
Detailed Insights
For a deeper understanding, consider the historical context, symptom progression, and ongoing research, which highlight the complexity of managing JIA effectively.
Comprehensive Report on Juvenile Idiopathic Arthritis (JIA)
This report provides an in-depth analysis of juvenile idiopathic arthritis (JIA), formerly known as juvenile rheumatoid arthritis, covering all essential aspects as requested. It is designed to be informative for both the general public and medical professionals, with detailed insights backed by credible sources.
Overview
JIA is defined as a chronic inflammatory disease affecting one or more joints in children under 16 years of age, with symptoms persisting for at least six weeks. It is the most common chronic rheumatic disease in children, with an estimated prevalence of approximately 50,000 children in the United States, and an annual incidence rate of 4-14 per 100,000 children. JIA is an autoimmune disorder, meaning the immune system mistakenly attacks the body’s own cells and tissues, leading to joint inflammation and potential involvement of other organs such as the heart, lungs, eyes, and nervous system.
Affected Body Parts/Organs:
- Joints: Any joint can be affected, with large joints like knees, ankles, and wrists being commonly involved.
- Eyes: Uveitis, an inflammation of the eye, is a frequent complication, particularly in certain subtypes like oligoarticular JIA.
- Internal Organs: In systemic-onset JIA, there can be inflammation of the heart (pericarditis), lungs (pleuritis), liver, spleen, and lymph nodes, which can have significant health implications.
Prevalence and Significance:
JIA’s prevalence varies globally, with estimates ranging from 3.8 to 400 per 100,000 children, reflecting differences in diagnostic criteria and population studies. Its significance lies in its potential to cause long-term morbidity, including joint deformity, growth disturbances, and visual impairment, underscoring the need for early diagnosis and treatment to mitigate these risks.
History & Discoveries
The first recorded description of a condition resembling JIA dates back to the 19th century, with Sir William Osler describing a case in 1895 of a 12-year-old girl with arthritis, fever, and rash, now recognized as systemic-onset JIA. The term “juvenile rheumatoid arthritis” was first used in the mid-20th century, and in 1995, it was renamed “juvenile idiopathic arthritis” to better define subgroups and distinguish it from adult rheumatoid arthritis, reflecting evolving medical understanding.
Major discoveries include the identification of different JIA subtypes based on clinical presentation and laboratory findings, the role of genetic factors like HLA-DR4 and HLA-DR8 in predisposing to certain types, and the development of effective treatments such as disease-modifying antirheumatic drugs (DMARDs) and biologics. These advancements have significantly improved disease control and outcomes, with a focus on early detection to prevent joint damage and other complications.
Symptoms
JIA presents with a variety of symptoms, varying by subtype, which can be categorized into early and advanced stages, as well as common and rare manifestations.
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms: Often include joint pain, swelling, and stiffness, particularly worse in the morning or after inactivity. Limping or reluctance to use a limb may be the first sign, especially in oligoarticular JIA. Systemic-onset JIA may present with high spiking fevers and a transient rash.
- Advanced-Stage Symptoms: Without treatment, joint damage can lead to deformity and disability, with possible growth disturbances affecting bone development. Chronic inflammation may result in joint erosion, and systemic cases can involve severe organ complications like pericarditis or pleuritis.
Common vs. Rare Symptoms:
- Common Symptoms: Across all types, joint pain, swelling, and stiffness are prevalent, along with morning stiffness and, in systemic cases, fever and rash.
- Rare Symptoms: Include internal organ involvement like hepatosplenomegaly or serositis in systemic-onset JIA, and asymptomatic uveitis, which requires regular screening to detect.
How Symptoms Progress Over Time:
Symptoms can fluctuate, with periods of flare and remission. Over time, without effective management, chronic inflammation can lead to irreversible joint damage, growth issues, and increased risk of complications like osteoporosis. Regular monitoring and early intervention are essential to manage progression and maintain quality of life.
Causes
The exact cause of JIA remains unknown, but it is believed to result from a complex interaction between genetic and environmental factors triggering an autoimmune response.
Biological and Environmental Causes:
- JIA is an autoimmune disease where the immune system attacks joint tissues, leading to inflammation. Environmental triggers, particularly viral infections, may initiate this response, though specific agents are not well-established. Other potential factors include exposure to certain toxins, but evidence is limited.
Genetic and Hereditary Factors:
- Genetic predisposition plays a significant role, with family history of autoimmune diseases increasing risk. Specific HLA genes, such as HLA-DR4 and HLA-DR8, are associated with certain JIA subtypes, and other genetic polymorphisms related to immune function have been identified, contributing to susceptibility.
Known Triggers or Exposure Risks:
- Infections, especially viral, are suspected triggers, potentially activating the immune system in genetically predisposed individuals. Gender also appears as a factor, with girls more commonly affected in some subtypes, though the mechanism is not fully understood.
Risk Factors
JIA’s risk factors include demographic, genetic, and environmental elements, given its onset in childhood.
Who is Most at Risk:
- Age: Onset is before 16 years, with peaks between 1-3 years and 9-12 years, reflecting developmental vulnerabilities.
- Gender: Girls are more affected, especially in oligoarticular and polyarticular subtypes, while boys are more commonly affected in enthesitis-related JIA, linked to HLA-B27.
- Occupation and Lifestyle: As a childhood disease, specific occupational risks are not applicable, but lifestyle factors like overall health and infection exposure may influence disease course.
Environmental, Occupational, and Genetic Factors:
- Environmental factors include potential infection exposure, though not occupation-specific. Genetic factors, such as family history and HLA types, significantly increase risk, with ethnicity also playing a role, as some subtypes are more prevalent in certain groups.
Impact of Pre-existing Conditions:
- Children with a family history of autoimmune diseases may have a higher risk, and pre-existing conditions like other immune dysregulation could exacerbate JIA, though specific data are limited.
Complications
JIA can lead to various complications, impacting long-term health and quality of life.
What Complications Can Arise:
- Joint Damage and Deformity: Chronic inflammation can erode cartilage and bone, leading to joint deformity and functional impairment.
- Growth Disturbances: Inflammation near growth plates can affect bone growth, causing limb length discrepancies or stunted growth.
- Uveitis: Eye inflammation can lead to vision loss if untreated, particularly in at-risk subtypes.
- Internal Organ Involvement: Systemic-onset JIA may involve pericarditis, pleuritis, hepatitis, or other organ inflammations, which can be severe and life-threatening.
- Osteoporosis: Chronic inflammation and corticosteroid use increase osteoporosis risk.
- Psychological and Social Impacts: Chronic disease can lead to depression, anxiety, and social isolation, affecting mental health and social development.
Long-term Impact on Organs and Overall Health:
- Long-term, JIA can result in permanent joint damage, growth issues, and organ dysfunction, particularly in systemic cases, potentially reducing life expectancy in severe instances.
Potential Disability or Fatality Rates:
- Disability rates vary, with effective treatment reducing long-term joint damage, but severe cases can lead to significant disability. Fatality is rare, primarily in systemic-onset JIA with severe organ involvement, with most children achieving a normal lifespan with proper management.
Diagnosis & Testing
Diagnosis of JIA relies on clinical criteria and supportive tests, with early detection being critical.
Common Diagnostic Procedures:
- Clinical Examination: Involves assessing joint swelling, pain, and range of motion, along with evaluating for extra-articular manifestations like rash or organomegaly.
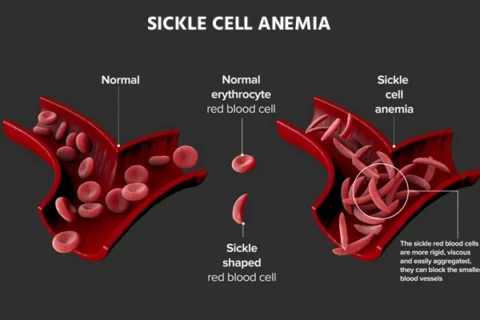
- Blood Tests: Include erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) for inflammation, rheumatoid factor (RF), and antinuclear antibodies (ANA) for subtype identification, and complete blood count (CBC) for anemia or other abnormalities.
- Imaging Studies: X-rays detect joint damage, while magnetic resonance imaging (MRI) provides detailed joint and soft tissue assessment.
- Ophthalmological Examination: Regular screening for uveitis, especially in at-risk children, is essential.
- Synovial Fluid Analysis: May be performed to rule out infection or other causes of joint inflammation.
Medical Tests:
- Blood tests and imaging are standard, with laboratory tests helping characterize the type of arthritis and rule out other conditions like infections or cancer.
Early Detection Methods and Their Effectiveness:
- Early detection involves regular follow-up and monitoring, with patient and parental education on recognizing symptoms. Effectiveness is high when combined with prompt treatment, preventing joint damage and complications, though asymptomatic uveitis can be challenging to detect without routine screening.
Treatment Options
Treatment aims to control inflammation, preserve joint function, and prevent complications, involving a multidisciplinary approach.
Standard Treatment Protocols:
- Goals include reducing pain, maintaining joint mobility, and preventing long-term damage, with regular monitoring and adjustment of therapy.
Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Used for pain and inflammation control, such as ibuprofen or naproxen.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Methotrexate, sulfasalazine, and leflunomide slow disease progression.
- Biologics: Tumor necrosis factor (TNF) inhibitors like etanercept, and interleukin-6 (IL-6) inhibitors like tocilizumab, for refractory cases.
- Corticosteroids: Oral or intra-articular injections, like prednisone, for severe inflammation, used cautiously due to side effects.
Surgeries and Therapies:
- Therapies: Physical therapy maintains joint mobility and strength, occupational therapy aids daily activities, and regular exercise supports fitness.
- Surgery: Joint replacement or corrective procedures for severe joint damage or deformity, though less common in children.
Emerging Treatments and Clinical Trials:
- Research is ongoing into new biologics targeting specific cytokines, personalized medicine based on genetic profiling, and non-invasive imaging for better disease assessment, with clinical trials exploring these innovations.
Prevention & Precautionary Measures
Given the unknown etiology, specific prevention is challenging, but measures can mitigate risks and manage disease.
How Can JIA Be Prevented?
- No definitive preventive measures exist, but early detection and treatment can prevent complications.
Lifestyle Changes and Environmental Precautions:
- Encouraging a balanced diet, regular exercise, and adequate rest supports overall health, potentially reducing disease impact. Avoiding known infection risks, like crowded environments during outbreaks, may help, though evidence is limited.
Vaccines or Preventive Screenings:
- Keeping up-to-date with vaccinations prevents infections that might trigger or exacerbate JIA. Regular ophthalmological exams are crucial for detecting uveitis early, a key preventive screening measure.
Global & Regional Statistics
JIA’s global and regional statistics highlight its variability and impact.
Incidence and Prevalence Rates Globally:
- Prevalence ranges from 3.8 to 400 per 100,000 children, with the US estimating about 50,000 affected children. Incidence is approximately 4-14 per 100,000 annually in the US, with variations due to diagnostic criteria and population differences.
Mortality and Survival Rates:
- Mortality is low, with most children achieving a normal lifespan, though severe systemic cases can be fatal. Survival rates are high with effective management, reflecting advances in treatment.
Country-wise Comparison and Trends:
- JIA is more common in regions like North America, Scandinavia, and parts of Europe, with higher prevalence in some Asian countries for systemic-onset JIA. Trends show increasing recognition and diagnosis, potentially due to improved awareness and diagnostic tools, though exact comparisons are limited by data availability.
Recent Research & Future Prospects
Recent advancements and ongoing studies offer hope for improved management and potential cures.
Latest Advancements in Treatment and Research:
- Biologics have revolutionized treatment, reducing the need for corticosteroids and improving outcomes. Genetic and immunological studies are identifying new therapeutic targets, enhancing personalized medicine approaches.
Ongoing Studies and Future Medical Possibilities:
- Research focuses on early biomarkers for prediction and monitoring, with clinical trials exploring new biologics and gene therapy. Non-invasive imaging techniques are being developed for better disease assessment, potentially leading to more effective, tailored treatments.
Potential Cures or Innovative Therapies Under Development:
- Future prospects include personalized medicine based on genetic profiling, novel biologics targeting specific cytokines, and possibly gene therapy to correct immune dysregulation, though these are still in early stages.
Interesting Facts & Lesser-Known Insights
JIA encompasses lesser-known aspects that enrich understanding and dispel myths.
Uncommon Knowledge About JIA:
- JIA is not a single disease but a group of conditions with seven subtypes, each with distinct features and outcomes. Some children may outgrow JIA, while others have lifelong disease, highlighting its variability.
Myths and Misconceptions vs. Medical Facts:
- Myth: JIA is the same as adult rheumatoid arthritis. Fact: It has distinct features, with different management strategies, reflecting its pediatric nature.
- Myth: JIA is caused by injury or poor parenting. Fact: It is an autoimmune disease with complex genetic and environmental factors, not lifestyle-related.
- Myth: Children with JIA cannot lead active lives. Fact: With proper management, they can participate in activities, supported by physical therapy and medication.
Impact on Specific Populations or Professions:
- JIA affects children worldwide, with varying prevalence by region, such as higher systemic-onset JIA in parts of Asia. Certain subtypes, like enthesitis-related JIA, are more common in boys and associated with HLA-B27, prevalent in some ethnic groups. Its impact on professions is minimal in childhood but can affect future career choices due to potential disability.
Tables
To enhance organization, the following tables summarize key aspects:
Table 1: JIA Subtypes and Common Symptoms
| Subtype | Common Symptoms | Notes |
|---|---|---|
| Oligoarticular JIA | Joint swelling, limp, asymmetrical | Most common, risk of uveitis |
| Polyarticular JIA | Multiple joint pain, morning stiffness | Can be RF-positive or negative |
| Systemic-Onset JIA | High fever, rash, organ involvement | Least common, can be severe |
| Enthesitis-Related JIA | Heel pain, lower back pain | More common in boys, HLA-B27 association |
| Psoriatic JIA | Arthritis, skin rash, nail changes | Associated with psoriasis |
Table 2: Treatment Options for JIA
| Category | Examples | Purpose |
|---|---|---|
| Medications (NSAIDs) | Ibuprofen, Naproxen | Pain and inflammation control |
| Medications (DMARDs) | Methotrexate, Sulfasalazine | Slow disease progression |
| Medications (Biologics) | Etanercept, Tocilizumab | Target specific immune responses, refractory cases |
| Therapies | Physical, Occupational Therapy | Maintain joint function, daily activity support |
| Surgery | Joint replacement | Correct severe joint damage or deformity |
Key Citations
- Juvenile Idiopathic Arthritis Detailed Overview [https://www.arthritis.org/diseases/juvenile-idiopathic-arthritis]
- National Institute Arthritis Juvenile Arthritis Info [https://www.niams.nih.gov/health-topics/juvenile-arthritis]
- Mayo Clinic Juvenile Idiopathic Arthritis Guide [https://www.mayoclinic.org/diseases-conditions/juvenile-idiopathic-arthritis/symptoms-causes/syc-20374082]
- American College Rheumatology Juvenile Arthritis [https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Juvenile-Arthritis]
- Pathogenesis Juvenile Rheumatoid Arthritis Study [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3012271/]