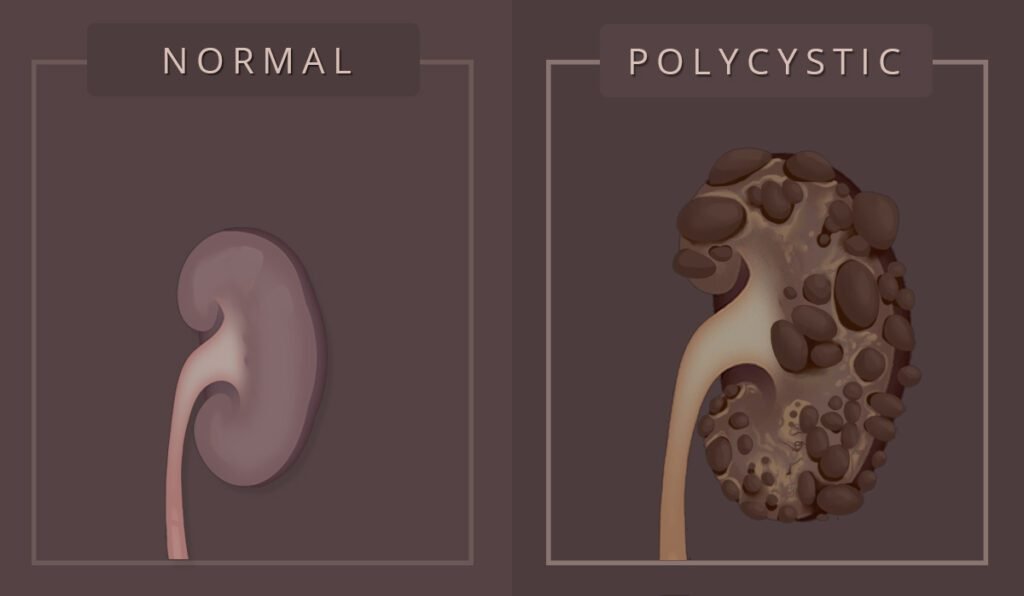
Polycystic kidney disease (PKD) is a group of inherited disorders characterized by the growth of multiple fluid‐filled cysts in the kidneys. Over time, the accumulation and expansion of these cysts can cause the kidneys to enlarge and lose their ability to function normally. PKD is one of the most common genetic disorders affecting the kidneys and is a significant cause of chronic kidney disease (CKD) and end‐stage renal disease (ESRD) worldwide. In this guide, we delve into every aspect of PKD—from definitions and genetic causes to the latest treatment options and supportive care.
1. Definition and Alternative Names
What Is Polycystic Kidney Disease?
Polycystic kidney disease is a genetic condition in which clusters of cysts develop primarily in the kidneys. These cysts are round, fluid-filled sacs that gradually enlarge over time. As cysts multiply and grow, they compress the normal kidney tissue, eventually impairing the kidney’s ability to filter blood effectively. In many cases, the progression leads to kidney failure. In addition to the kidneys, cysts may also form in other organs, including the liver, pancreas, and even the heart or brain in some instances.
Alternative Names
Polycystic kidney disease is known by several other names, reflecting its genetic and clinical heterogeneity:
- PKD: A common abbreviation.
- Polycystic renal disease: Emphasizes the kidney involvement.
- Autosomal dominant polycystic kidney disease (ADPKD): The most common inherited form, typically diagnosed in adulthood.
- Autosomal recessive polycystic kidney disease (ARPKD): A rarer form that generally presents in infancy or early childhood.
- Adult-onset PKD: Another term for ADPKD.
- Inherited cystic kidney disease: A broader term that can also include less common inherited cystic conditions.
Understanding these alternative names is important because they sometimes guide the discussion of treatment, prognosis, and genetic counseling.
2. Epidemiology and Classification
How Common Is PKD?
PKD is one of the most common inherited kidney disorders. It is estimated that approximately 600,000 people in the United States live with PKD. Globally, autosomal dominant polycystic kidney disease (ADPKD) affects about 1 in 500 to 1 in 1,000 individuals, while autosomal recessive PKD (ARPKD) is much less common, affecting approximately 1 in 20,000 to 40,000 live births.
Both forms affect individuals of all races and genders, although ADPKD is usually diagnosed in adults between the ages of 30 and 40, whereas ARPKD tends to present earlier—in infancy or early childhood.
Classification of PKD
Polycystic kidney disease is classified into three primary types:
Autosomal Dominant Polycystic Kidney Disease (ADPKD):
- Inheritance: Autosomal dominant; only one copy of the mutated gene (from one affected parent) is required for the disease to develop.
- Onset: Typically begins in adulthood, though cysts may be present from birth.
- Prevalence: It accounts for about 90% of PKD cases.
- Genetics: Mainly caused by mutations in the PKD1 gene (approximately 85% of cases) or PKD2 gene (approximately 15% of cases). Recent research has also identified a less common form, sometimes referred to as PKD3, associated with mutations in the GANAB gene.
Autosomal Recessive Polycystic Kidney Disease (ARPKD):
- Inheritance: Autosomal recessive; both parents must carry and pass on a mutated copy of the gene (commonly the PKHD1 gene) for the child to be affected.
- Onset: Presents in the perinatal period, infancy, or early childhood.
- Severity: Generally more severe than ADPKD; often associated with early kidney failure and congenital hepatic fibrosis.
Acquired Cystic Kidney Disease (ACKD):
- Nature: Not inherited but develops in individuals with chronic kidney disease, especially those on long-term dialysis.
- Features: Characterized by the formation of multiple cysts in kidneys that have already been damaged by other diseases.
Each type has unique genetic underpinnings, clinical courses, and management strategies, making accurate diagnosis and classification crucial.
3. Causes and Genetic Basis
Genetic Causes
PKD is primarily a genetic disorder, meaning that it is caused by mutations in specific genes. The mode of inheritance and the type of gene involved help determine the severity and age of onset of the disease.
Autosomal Dominant PKD (ADPKD)
PKD1 Gene:
- Location: Chromosome 16
- Prevalence: Accounts for approximately 85% of ADPKD cases.
- Protein Function: Encodes polycystin-1, a protein involved in cell–cell and cell–matrix interactions, and plays a role in the development and function of renal tubules.
- Clinical Course: Mutations in PKD1 tend to result in a more severe disease with an earlier onset of kidney failure compared to PKD2 mutations.
PKD2 Gene:
- Location: Chromosome 4
- Prevalence: Accounts for about 15% of ADPKD cases.
- Protein Function: Encodes polycystin-2, which functions as a calcium-permeable ion channel. It interacts with polycystin-1 to regulate intracellular calcium levels.
- Clinical Course: Generally associated with a milder form of the disease and later onset of kidney failure.
PKD3 / GANAB:
- Recent Research: Some families have been identified with ADPKD that do not have mutations in PKD1 or PKD2 but instead in GANAB. These mutations may also lead to cyst formation and can be associated with polycystic liver disease.
- Significance: Although less common, these cases underscore the genetic heterogeneity of ADPKD.
Autosomal Recessive PKD (ARPKD)
- PKHD1 Gene:
- Location: Chromosome 6p12.2
- Prevalence: Responsible for virtually all cases of ARPKD.
- Protein Function: Encodes fibrocystin (also known as polyductin), which is expressed in the kidney and liver. The protein plays a crucial role in the development of renal tubules and bile ducts.
- Clinical Course: ARPKD typically presents in the perinatal period with severe kidney dysfunction, and in many cases, it leads to early mortality or progression to kidney failure in childhood.
Non-Genetic and Acquired Factors
While PKD is predominantly genetic, a subset of cystic kidney diseases is acquired. Acquired cystic kidney disease (ACKD) is typically seen in patients with chronic kidney disease or those who have been on dialysis for several years. The exact mechanism is not fully understood, but it is believed that long-term dialysis and chronic kidney injury lead to cyst formation.
Risk Factors
- Family History: The most significant risk factor, particularly in ADPKD.
- Age: Symptoms of ADPKD often develop between 30 and 40 years of age.
- Ethnicity and Gender: ADPKD affects both genders equally, while ARPKD affects infants regardless of gender.
- Other Conditions: Chronic kidney disease from other causes can predispose to acquired cystic kidney disease.
Understanding the genetic and molecular basis of PKD has been critical for developing targeted therapies and for providing genetic counseling to families affected by this condition.
4. Pathophysiology
The pathophysiology of PKD involves complex mechanisms that lead to cyst formation and progressive loss of kidney function.
Cyst Formation
Initiation:
In ADPKD, cysts typically begin as small dilations in the renal tubules. A “two-hit” hypothesis is widely accepted: an individual inherits one mutated copy of the gene (first hit) and then later acquires a somatic mutation in the normal allele (second hit). This loss of heterozygosity triggers abnormal cell proliferation and cyst formation.Growth and Expansion:
Once initiated, the cysts grow in size due to fluid accumulation. The fluid secretion into the cysts is driven by increased cyclic adenosine monophosphate (cAMP) levels, which promote both cell proliferation and chloride-driven fluid secretion. Over time, these cysts can become large and numerous, replacing normal renal parenchyma and interfering with kidney function.
Molecular Mechanisms
Polycystin-1 and Polycystin-2:
In ADPKD, the proteins produced by the PKD1 and PKD2 genes are crucial for maintaining the normal structure and function of renal tubules. These proteins are localized to the primary cilium, a sensory organelle on the surface of renal tubular cells. They regulate calcium signaling, which in turn influences cell proliferation and fluid secretion. Defects in these proteins disrupt intracellular calcium homeostasis, leading to increased cAMP levels and cyst growth.Fibrocystin/Polyductin:
In ARPKD, mutations in PKHD1 lead to defects in fibrocystin, a protein essential for the normal development of renal tubules and bile ducts. Loss of fibrocystin function results in the formation of cysts not only in the kidneys but also in the liver, often leading to congenital hepatic fibrosis.
Consequences of Cyst Growth
- Loss of Functional Kidney Tissue:
As cysts enlarge, they compress and replace normal kidney tissue, leading to a reduction in the number of functional nephrons. - Activation of the Renin-Angiotensin-Aldosterone System (RAAS):
Reduced kidney function and tissue ischemia can activate the RAAS, further contributing to high blood pressure (hypertension) and worsening kidney damage. - Progressive Renal Failure:
Eventually, the loss of functional kidney tissue leads to chronic kidney disease and, ultimately, end-stage renal disease (ESRD), necessitating renal replacement therapies such as dialysis or kidney transplantation.
These molecular and cellular mechanisms not only explain the progression of PKD but also provide targets for therapeutic intervention, as discussed in later sections.
5. Signs and Symptoms
Early Symptoms
The early clinical manifestations of PKD can be subtle, which is why many individuals remain unaware of their condition until later in life:
- High Blood Pressure (Hypertension):
One of the most common early signs, often detected during routine physical examinations. - Flank or Back Pain:
Dull, intermittent pain that may be caused by the growth of cysts or bleeding within a cyst. - Abdominal Fullness or Bloating:
As the kidneys enlarge due to cyst growth, patients may notice an increase in abdominal girth. - Hematuria (Blood in the Urine):
Occasional episodes of blood in the urine, often painless. - Urinary Tract Infections (UTIs):
Frequent infections can occur as cysts become infected.
Progressive Symptoms
As PKD advances, symptoms become more pronounced and may include:
- Persistent or Worsening Pain:
Pain in the sides, back, or abdomen can intensify as cysts grow larger. - Recurrent UTIs and Kidney Infections:
Infections can become more frequent and severe, potentially leading to sepsis. - Kidney Stones:
The presence of stones may occur, leading to sharp, colicky pain. - Decreased Kidney Function:
As the disease progresses, laboratory tests may reveal worsening kidney function, eventually leading to chronic kidney disease or kidney failure. - Liver Cysts:
Many patients, particularly those with ADPKD, develop cysts in the liver, which usually do not affect liver function but can sometimes cause discomfort or complications. - Aneurysms:
There is an increased risk of developing aneurysms (particularly in the brain), which may be asymptomatic until rupture. - Cardiac Complications:
High blood pressure and chronic kidney disease may lead to heart valve abnormalities or heart failure over time.
Signs in Children (ARPKD)
Children with autosomal recessive polycystic kidney disease often present with:
- Enlarged, Abnormal Kidneys:
Detected prenatally or soon after birth by ultrasound. - High Blood Pressure:
Even in early infancy. - Failure to Thrive:
Poor growth and developmental delays. - Respiratory Distress:
In severe cases, due to oligohydramnios (low amniotic fluid) affecting lung development (Potter sequence).
Because the onset and severity of symptoms vary widely, regular monitoring is essential—especially if there is a known family history of PKD.
6. Diagnostic Exams and Tests
Diagnosing PKD typically involves a combination of a thorough medical history, physical examination, laboratory tests, and imaging studies.
Medical History and Physical Examination
- Family History:
Since PKD is mostly inherited, documenting a family history of kidney disease, high blood pressure, or kidney failure is critical. - Physical Exam:
The doctor may detect an enlarged abdomen or palpable masses in the flanks (enlarged kidneys). Blood pressure is routinely checked because hypertension is a common early sign.
Laboratory Tests
- Blood Tests:
These include assessments of kidney function such as serum creatinine, blood urea nitrogen (BUN), and estimated glomerular filtration rate (eGFR). A complete blood count (CBC) can detect anemia, which is common in kidney disease. - Urinalysis:
This test is used to check for the presence of blood, protein, or bacteria in the urine, all of which may be associated with PKD. - Liver Function Tests:
Since PKD can also affect the liver, these tests are sometimes performed.
Imaging Studies
Imaging is the cornerstone of PKD diagnosis:
1. Ultrasound
- Primary Diagnostic Tool:
Ultrasound is inexpensive, noninvasive, and highly effective for detecting cysts in the kidneys. In at-risk individuals (especially those over 40), a normal ultrasound usually rules out ADPKD. - Monitoring:
It is also used to monitor cyst growth and kidney size over time.
2. Computed Tomography (CT) Scan
- High-Resolution Imaging:
CT scans provide detailed images of the kidneys and are useful for detecting smaller cysts that might not be seen on ultrasound. - Volume Measurement:
CT imaging can be used to calculate total kidney volume (TKV), which has prognostic significance.
3. Magnetic Resonance Imaging (MRI)
- Detailed Visualization:
MRI is especially useful for measuring kidney and cyst volumes and is often used in clinical research to monitor disease progression. - No Radiation:
Unlike CT scans, MRI does not expose patients to ionizing radiation, making it a safer choice for repeated assessments.
4. Intravenous Pyelogram (IVP)
- Contrast Imaging:
Although less commonly used now, IVP involves injecting a contrast dye and taking X-ray images to visualize the urinary tract.
Genetic Testing
- Role in Diagnosis:
Genetic testing can confirm the diagnosis, particularly in families with a known history of PKD. However, it is not necessary for all patients due to cost and a detection failure rate of approximately 15%. - Indications:
It is especially useful when imaging results are inconclusive, for young individuals with a family history, or for potential kidney donors from affected families.
Additional Assessments
- Blood Pressure Monitoring:
Regular monitoring is essential, as hypertension is both a symptom and a contributor to disease progression. - Assessment for Extrarenal Manifestations:
Given that PKD can affect other organs (liver, pancreas, brain aneurysms), additional imaging studies like liver ultrasound or cerebral angiography may be recommended in certain cases.
A multidisciplinary approach to diagnosis helps ensure that all aspects of PKD are identified and managed early.
7. Treatment Options
Currently, there is no cure for polycystic kidney disease; treatment is aimed at managing symptoms, slowing progression, and preventing complications. Management strategies differ based on the type of PKD (ADPKD, ARPKD, or ACKD) and the severity of the disease.
7.1. Lifestyle and Dietary Management
Healthy Diet:
- Low-Sodium Diet: Reducing salt intake can help manage high blood pressure, which is crucial for slowing kidney damage.
- Moderate Protein: While protein is necessary, excessive protein intake may accelerate kidney damage. A dietician specializing in kidney disease can provide personalized advice.
- Hydration: Adequate fluid intake may help dilute the urine and slow cyst growth. Some research suggests that increasing water intake may reduce levels of vasopressin (antidiuretic hormone), which in turn may slow cyst expansion.
Exercise:
- Regular Physical Activity: Moderate exercise helps manage blood pressure, reduce stress, and maintain overall health. However, contact sports that risk trauma to the kidneys should be avoided.
- Weight Management: Achieving and maintaining a healthy weight reduces the burden on the kidneys and can help control blood pressure.
Smoking Cessation and Limiting Alcohol:
- Avoid Smoking: Smoking is a risk factor for kidney damage and cardiovascular disease.
- Limit Alcohol Intake: Excessive alcohol can exacerbate high blood pressure and impair kidney function.
7.2. Medications
Medications in PKD are primarily aimed at controlling blood pressure and managing pain or complications.
Antihypertensives:
- ACE Inhibitors/ARBs: These medications help control blood pressure and have been shown to slow the progression of kidney damage. They are often the first-line treatment in patients with PKD.
- Beta-Blockers and Calcium Channel Blockers: These can be used in certain cases, depending on the patient’s overall cardiovascular profile.
Pain Management:
- Acetaminophen: Generally recommended for pain relief.
- Avoid NSAIDs: Nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen) can worsen kidney function and are usually avoided in patients with PKD.
Cyst Management:
- Tolvaptan: Approved by the FDA in 2018 (brand name Jynarque) for ADPKD, tolvaptan is a vasopressin V2 receptor antagonist that can slow kidney function decline and reduce cyst growth. Regular monitoring of liver function is necessary due to the risk of liver injury.
- Antibiotics: Prompt treatment of urinary tract or kidney infections is critical to prevent further kidney damage.
- Sclerotherapy or Cyst Drainage: In cases where cysts cause significant pain or discomfort, drainage of cyst fluid or injection of sclerosing agents may be performed.
- Management of Complications: Treatments for kidney stones, urinary tract infections, and other complications are tailored to the individual’s needs.
7.3. Advanced Treatments
Dialysis:
- When kidney function declines significantly, patients may require renal replacement therapy.
- Hemodialysis and Peritoneal Dialysis: Both modalities are used, with the choice depending on patient factors, kidney size, and overall health.
Kidney Transplantation:
- Transplantation: Kidney transplant is the definitive treatment for end-stage renal disease (ESRD) resulting from PKD.
- Preemptive Transplantation: Some patients may be candidates for kidney transplant before the onset of full kidney failure, which can improve outcomes.
- Native Nephrectomy: In cases where the kidneys are extremely enlarged and symptomatic, removal of the native kidneys may be performed in conjunction with transplantation.
7.4. Emerging and Experimental Therapies
Research is ongoing to find therapies that can halt or even reverse cyst growth. Some promising areas include:
- Dietary Interventions:
- Ketogenic Diet: Preliminary studies in animal models and small human case series suggest that ketogenic or calorie-restricted diets may slow cyst growth.
- Time-Restricted Feeding: Early research indicates that limiting food intake to specific times of the day could have beneficial effects on cyst progression.
- Novel Medications:
- Research is exploring agents that target specific molecular pathways (such as mTOR inhibitors and agents affecting cAMP signaling) involved in cyst growth.
- Genetic Therapies:
- Although still in early stages, future gene-targeted therapies may offer a cure by correcting the underlying genetic defect.
Together, these therapies represent a multi-pronged approach to managing PKD, with the goal of preserving kidney function for as long as possible and improving quality of life.
8. Support Groups and Resources
Living with polycystic kidney disease can be challenging both physically and emotionally. Fortunately, several organizations and online communities provide support, advocacy, and up-to-date information for patients and families:
National Organizations
- PKD Foundation:
- Provides comprehensive resources for patients and families, including education, advocacy, and support networks.
- Offers local chapters and events to help patients connect.
- National Kidney Foundation (NKF):
- Offers educational materials, support groups, and community events.
- Provides guidance on managing kidney disease and preparing for kidney replacement therapies.
- National Organization for Rare Disorders (NORD):
- Offers resources and advocacy for rare diseases, including PKD.
- American Association of Kidney Patients (AAKP):
- Provides patient education, advocacy, and community support.
Online Communities and Forums
- Mayo Clinic Connect:
- An online patient community where people with PKD can share experiences, ask questions, and support each other.
- HealthUnlocked and Inspire:
- Platforms that host dedicated PKD groups for patients and caregivers.
- Social Media Groups:
- Facebook and Twitter have active communities where patients, families, and caregivers exchange information and advice.
Genetic Counseling Services
For individuals with a family history of PKD who are considering having children, genetic counseling is an important resource. Genetic counselors can help you understand inheritance patterns, assess risks, and discuss options for prenatal testing.
Educational Resources
- Mayo Clinic, Johns Hopkins Medicine, and Penn Medicine:
- Provide detailed, up-to-date information on PKD, treatment options, and lifestyle modifications.
- MedlinePlus and NIDDK:
- Offer reliable information on the genetics, diagnosis, and management of PKD.
- Peer-Reviewed Journals and Clinical Guidelines:
- For those interested in the latest research, resources like the New England Journal of Medicine, Kidney International, and Clinical Journal of the American Society of Nephrology provide in-depth studies and reviews.
Connecting with these resources can be an essential part of managing the disease and coping with its challenges.
9. Prognosis
Overview of Disease Progression
The course of polycystic kidney disease is highly variable. In ADPKD, cysts often begin forming in childhood; however, symptoms typically do not appear until adulthood. Kidney function may remain relatively normal for many years, but gradual cyst expansion eventually leads to loss of functional kidney tissue.
- End-Stage Renal Disease (ESRD):
- Approximately 50% of patients with ADPKD will develop kidney failure by age 60, and about 60% by age 70.
- ESRD requires renal replacement therapy, such as dialysis or kidney transplantation.
Factors Influencing Prognosis
Several factors can affect the rate of disease progression and overall prognosis:
- Genetic Mutation Type:
- Patients with PKD1 mutations tend to have an earlier onset and more aggressive disease compared to those with PKD2 mutations.
- Total Kidney Volume (TKV):
- TKV, particularly when adjusted for patient height (HtTKV), is an important predictor of disease progression. Studies have shown that larger kidney volumes correlate with a more rapid decline in kidney function.
- Blood Pressure Control:
- Hypertension is a major contributor to kidney damage in PKD. Effective blood pressure management can slow disease progression.
- Lifestyle Factors:
- Diet, exercise, and avoiding harmful substances (like tobacco) can influence disease progression.
- Extrarenal Manifestations:
- The presence of cysts in the liver, pancreas, or aneurysms in the brain can complicate the disease course.
Prognostic Models
Recent research has focused on developing prognostic models using imaging data (e.g., TKV) and clinical markers (e.g., eGFR, blood pressure) to predict which patients are at higher risk of rapid progression. One widely used model is based on the Mayo imaging classification, which categorizes patients into subclasses based on kidney volume relative to age. This information helps physicians tailor treatment strategies and monitor high-risk patients more closely.
While there is no cure for PKD, early detection and proactive management can substantially improve quality of life and slow the progression to kidney failure.
10. Possible Complications
Complications of PKD can affect multiple organ systems, and their severity may vary widely among patients.
Renal Complications
- Hypertension:
- High blood pressure is nearly universal in PKD patients and is a significant contributor to kidney damage.
- Chronic Kidney Disease (CKD) and ESRD:
- Progressive loss of kidney function eventually leads to kidney failure, necessitating dialysis or transplantation.
- Kidney Stones:
- Cysts may predispose to the formation of kidney stones, leading to pain and possible urinary obstruction.
- Infections:
- Cysts can become infected, leading to recurrent urinary tract infections or even sepsis.
- Cyst Hemorrhage:
- Bleeding into cysts can cause sudden flank pain and hematuria.
Extrarenal Complications
- Liver Cysts and Polycystic Liver Disease:
- Many patients with ADPKD develop cysts in the liver, which may cause abdominal discomfort or, in rare cases, impair liver function.
- Intracranial Aneurysms:
- There is an increased risk of aneurysm formation in cerebral vessels, which can rupture and cause subarachnoid hemorrhage.
- Cardiovascular Complications:
- Long-standing hypertension increases the risk of heart disease, including left ventricular hypertrophy and heart failure.
- Mitral Valve Prolapse:
- Abnormalities in heart valves, particularly the mitral valve, are seen in some patients.
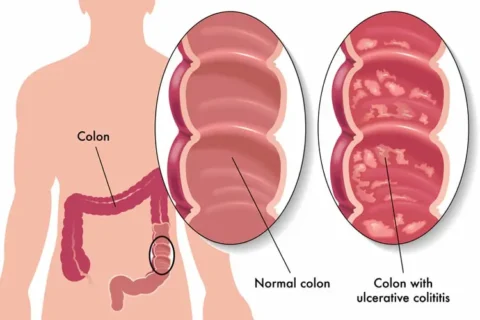
- Colonic Diverticulosis:
- The formation of pouches in the colon wall may occur, which can lead to pain or bleeding.
These complications underscore the importance of regular monitoring and early intervention to manage both renal and extrarenal manifestations of PKD.
11. When to Seek Medical Attention
Prompt medical attention is important when symptoms or complications of PKD arise. You should contact your healthcare provider if you experience any of the following:
- Persistent or Worsening Flank/Abdominal Pain:
- Pain may indicate cyst rupture, hemorrhage, or infection.
- Sudden Onset of Blood in the Urine (Hematuria):
- While minor episodes can resolve on their own, significant or recurrent hematuria warrants evaluation.
- High Blood Pressure:
- Uncontrolled hypertension can accelerate kidney damage; regular blood pressure monitoring is essential.
- Signs of Infection:
- Fever, chills, or discomfort in the kidney area may signal a urinary tract or cyst infection.
- Changes in Kidney Function:
- Symptoms such as fatigue, decreased urine output, or swelling in the legs may indicate declining kidney function.
- Neurological Symptoms:
- Severe headaches, visual changes, or neurological deficits could suggest the presence or rupture of an intracranial aneurysm.
- Pregnancy Concerns:
- Women with PKD should consult their healthcare provider about the risks and necessary monitoring during pregnancy, particularly if they have high blood pressure or reduced kidney function.
Early evaluation by a nephrologist or a kidney specialist can help manage complications before they become life-threatening.
12. Preventive Measures
While you cannot prevent the genetic mutation that causes PKD, there are several strategies to help slow disease progression and prevent complications:
Lifestyle Modifications
- Blood Pressure Control:
- Regular monitoring and treatment with antihypertensive medications (such as ACE inhibitors or ARBs) are crucial to protect kidney function.
- Healthy Diet:
- Follow a diet low in sodium to manage blood pressure and reduce fluid retention.
- Moderate protein intake is recommended to avoid overburdening the kidneys.
- Staying well hydrated may help reduce cyst growth, though your fluid intake should be personalized based on your overall kidney function.
- Regular Exercise:
- Engage in moderate physical activity, such as walking or swimming, to improve cardiovascular health and overall well-being. Avoid high-impact activities that could injure the kidneys.
- Weight Management:
- Maintaining a healthy weight reduces the strain on your kidneys and helps control blood pressure.
- Avoid Smoking and Excessive Alcohol:
- Smoking and excessive alcohol intake can exacerbate kidney damage and worsen hypertension.
- Stress Management:
- Chronic stress can contribute to high blood pressure. Techniques such as mindfulness, yoga, and counseling can be beneficial.
Medical Management
- Regular Check-Ups:
- Frequent monitoring of kidney function through blood tests (e.g., serum creatinine, eGFR) and imaging studies helps detect changes early.
- Genetic Counseling:
- If you have a family history of PKD and are planning to have children, genetic counseling can help assess risks and discuss reproductive options.
- Infection Prevention:
- Prompt treatment of urinary tract infections and cyst infections is essential to prevent further kidney damage.
- Vaccinations:
- Stay up to date on recommended vaccines (e.g., influenza, pneumonia) to prevent infections that could stress the kidneys.
Emerging Strategies
Research into novel dietary interventions—such as ketogenic diets, time-restricted feeding, and caloric restriction—is ongoing. Some early studies in animal models and small human trials have shown promise in slowing cyst growth. Although these strategies are not yet standard care, they highlight the importance of further research and individualized dietary counseling.
By combining these preventive measures, patients with PKD can help slow the progression of the disease, reduce the risk of complications, and maintain a higher quality of life for a longer period.