Definition and Alternative Names
What Is COPD?
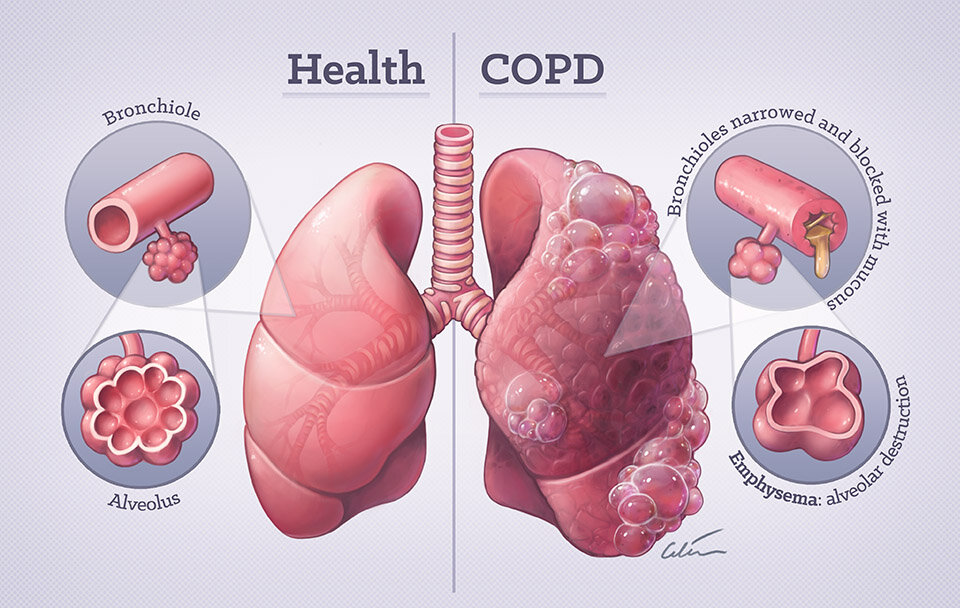
Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable, and treatable lung disease characterized by persistent respiratory symptoms and airflow limitation that is usually progressive. The airflow limitation in COPD is due to a mixture of small airway disease (e.g., chronic bronchitis) and parenchymal destruction (emphysema). These pathological changes lead to breathing difficulties, chronic cough, and sputum production.
Alternative Names and Terminology
COPD is an umbrella term that covers several conditions:
- Chronic Bronchitis: Involves inflammation and narrowing of the bronchial tubes along with excessive mucus production. Clinically, it is defined as a productive cough lasting at least three months per year for two consecutive years.
- Emphysema: Characterized by the destruction of the alveoli (air sacs) in the lungs, which results in impaired gas exchange and reduced lung elasticity.
- Chronic Obstructive Lung Disease (COLD): Another term sometimes used, especially in European countries.
- Obstructive Lung Disease: A broader term that can include asthma; however, COPD is distinct in its chronic and progressive nature.
Regardless of the specific term, all these conditions share the common feature of airflow obstruction, which is not fully reversible.
2. Epidemiology and Public Health Importance
Prevalence and Demographics
COPD is one of the leading causes of morbidity and mortality globally. According to the World Health Organization (WHO), COPD is the third leading cause of death worldwide. In the United States alone, an estimated 16 million people have been diagnosed with COPD, though many more may be undiagnosed. The disease predominantly affects older adults, typically those aged 40 and above, and has a higher prevalence among individuals with a history of smoking.
Economic and Social Impact
COPD places a significant burden on healthcare systems due to frequent hospitalizations, long-term treatments, and the need for supportive care. The disease not only affects the individual’s physical health but also has substantial socioeconomic implications, including reduced work productivity and increased healthcare expenditures.
Public Health Importance
Early recognition, preventive strategies, and effective management are critical to reducing the burden of COPD. Public health initiatives that promote smoking cessation, air quality improvement, and vaccination against respiratory infections are essential components in the fight against COPD.
3. Causes and Risk Factors
Major Causes
The primary cause of COPD is long-term exposure to irritating gases or particulate matter that damages the lungs and the airways. The most common risk factors include:
3.1. Smoking
- Cigarette Smoking:
- Smoking is by far the most significant risk factor for COPD. It accounts for approximately 85-90% of COPD cases. The toxic chemicals in cigarette smoke cause chronic inflammation in the airways and lung tissue, leading to structural changes.
- Other Forms of Tobacco:
- Use of cigars, pipes, and other tobacco products also increases the risk.
- Secondhand Smoke:
- Exposure to secondhand smoke can also contribute to the development of COPD.
3.2. Environmental and Occupational Exposures
- Air Pollution:
- Long-term exposure to outdoor air pollution, including industrial emissions, vehicle exhaust, and dust, is associated with COPD.
- Occupational Hazards:
- Jobs that expose workers to dust, chemicals, and fumes (e.g., mining, construction, agriculture) increase the risk.
- Indoor Air Pollution:
- In developing countries, burning biomass fuels (wood, crop residues, dung) for cooking and heating in poorly ventilated spaces is a significant risk factor.
3.3. Genetic Factors
- Alpha-1 Antitrypsin Deficiency:
- A small percentage of COPD cases (approximately 1-3%) are due to a genetic disorder called alpha-1 antitrypsin deficiency. This condition leads to a deficiency of alpha-1 antitrypsin, a protein that protects the lungs from inflammation caused by infections or irritants.
3.4. Other Risk Factors
- Age:
- COPD is more common in individuals over the age of 40.
- Gender:
- Historically, COPD was more prevalent in men due to higher smoking rates; however, the gap has narrowed, and women are increasingly affected.
- Respiratory Infections:
- Severe respiratory infections during childhood may predispose individuals to COPD later in life.
- Socioeconomic Status:
- Lower socioeconomic status is associated with higher COPD risk, partly due to increased exposure to pollutants and reduced access to healthcare.
Summary
While cigarette smoking remains the most significant contributor to COPD, a combination of environmental exposures, genetic predisposition, and other factors also plays a role in its development. Understanding these risk factors is critical for both prevention and management.
4. Pathophysiology
The pathophysiology of COPD involves complex inflammatory processes that lead to structural changes in the airways and lung tissue.
4.1. Chronic Inflammation
- Inflammatory Response:
- Inhaled irritants such as cigarette smoke trigger an inflammatory response in the lungs. This response involves the activation of immune cells (neutrophils, macrophages, T-lymphocytes) that release cytokines and proteolytic enzymes.
- Tissue Damage:
- The chronic inflammation results in damage to the alveolar walls (in emphysema) and thickening of the bronchial walls (in chronic bronchitis).
4.2. Airflow Limitation
- Obstructive Component:
- In COPD, the airflow limitation is both due to small airway disease (bronchiolitis) and destruction of lung parenchyma (emphysema). The loss of elastic recoil in emphysema and airway narrowing in chronic bronchitis combine to reduce airflow, particularly during exhalation.
- Air Trapping:
- The reduction in airflow leads to air trapping in the lungs, which causes hyperinflation, increased work of breathing, and reduced gas exchange.
4.3. Structural Changes in the Lungs
- Emphysema:
- Characterized by the destruction of alveolar walls, emphysema reduces the surface area available for gas exchange and impairs oxygen uptake.
- Chronic Bronchitis:
- In chronic bronchitis, the airways are inflamed and produce excessive mucus, which obstructs the airways and predisposes to infections.
4.4. Systemic Effects
- Cardiovascular Impact:
- The chronic low oxygen levels and systemic inflammation associated with COPD can contribute to the development of cardiovascular disease, including pulmonary hypertension and right-sided heart failure (cor pulmonale).
- Skeletal Muscle Dysfunction:
- Chronic hypoxia and systemic inflammation can lead to muscle wasting and decreased exercise capacity.
Summary
The interplay of chronic inflammation, structural changes in the lung tissue, and airflow limitation underlies the clinical manifestations of COPD. These pathophysiological processes not only impair respiratory function but also contribute to the systemic complications associated with the disease.
5. Symptoms of COPD
COPD is characterized by a range of symptoms that vary in severity and progression. Understanding these symptoms is key to early diagnosis and effective management.
5.1. Respiratory Symptoms
- Chronic Cough:
- A persistent cough is common, often accompanied by sputum production. In chronic bronchitis, the cough is typically productive and may be worse in the morning.
- Dyspnea (Shortness of Breath):
- Initially, shortness of breath may occur only during exertion but can progress to occur even at rest in advanced stages.
- Wheezing:
- A whistling sound during breathing may be present, especially during episodes of exacerbation.
- Chest Tightness:
- Some patients experience a feeling of tightness or discomfort in the chest.
5.2. Systemic Symptoms
- Fatigue and Reduced Exercise Capacity:
- The increased work of breathing and reduced oxygenation can lead to chronic fatigue and a significant decrease in physical stamina.
- Frequent Respiratory Infections:
- Patients with COPD are more susceptible to infections such as bronchitis and pneumonia.
- Weight Loss and Muscle Wasting:
- In advanced COPD, unintentional weight loss and muscle wasting (cachexia) may occur due to chronic hypoxia and systemic inflammation.
- Cyanosis:
- A bluish tint to the lips or skin may be seen in severe cases, indicating inadequate oxygenation.
- Swelling (Edema):
- In some patients, particularly those with right heart failure (cor pulmonale), swelling of the ankles and legs may occur.
5.3. Variability in Presentation
The severity and frequency of symptoms can vary considerably between patients. Early in the disease, symptoms might be mild and intermittent, leading many patients to underestimate their condition. As COPD progresses, however, symptoms tend to become more persistent and disabling, impacting daily activities and overall quality of life.
6. Diagnostic Exams and Tests
A thorough diagnostic workup is essential to confirm COPD and assess its severity. Diagnosis is primarily based on clinical evaluation and is supported by several key diagnostic tests.
6.1. Medical History and Physical Examination
- History:
- A detailed history of smoking (including duration and intensity) is crucial.
- Symptoms such as chronic cough, sputum production, and dyspnea are documented.
- Occupational exposures, family history of lung disease, and previous respiratory infections are also considered.
- Physical Examination:
- The healthcare provider listens to the lungs for wheezing, crackles, or diminished breath sounds.
- Inspection of the chest may reveal signs of hyperinflation.
- Evaluation for signs of right heart failure (e.g., peripheral edema, jugular venous distension) is performed.
6.2. Spirometry
Spirometry is the cornerstone of COPD diagnosis:
- Forced Expiratory Volume in 1 Second (FEV₁):
- Measures the volume of air exhaled in the first second of a forceful breath.
- Forced Vital Capacity (FVC):
- Total volume of air that can be forcefully exhaled.
- FEV₁/FVC Ratio:
- In COPD, this ratio is reduced (typically less than 70%), indicating airflow obstruction.
- Bronchodilator Response:
- Repeating spirometry after administering a bronchodilator helps assess reversibility; a lack of significant improvement supports a diagnosis of COPD rather than asthma.
6.3. Imaging Studies
- Chest X-Ray:
- Can reveal hyperinflated lungs, flattened diaphragms, and increased retrosternal airspace. It also helps rule out other causes of respiratory symptoms.
- Computed Tomography (CT) Scan:
- Provides detailed images of lung parenchyma, helping to assess emphysematous changes and detect complications such as lung cancer.
- High-Resolution CT (HRCT):
- Particularly useful in evaluating the extent and distribution of emphysema and airway remodeling.
6.4. Laboratory Tests
- Arterial Blood Gas (ABG):
- Assesses oxygenation and carbon dioxide retention, which is critical in advanced COPD.
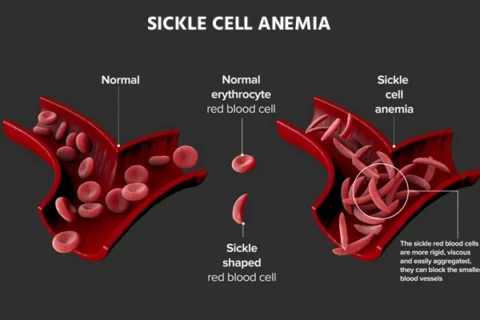
- Complete Blood Count (CBC):
- Can detect polycythemia (an increased red blood cell count), which may be a compensatory response to chronic hypoxemia.
- Biomarkers:
- Levels of certain inflammatory markers may be evaluated in research settings but are not yet routine.
6.5. Additional Diagnostic Tests
- Six-Minute Walk Test:
- Measures exercise tolerance and oxygen desaturation during exertion. This test is useful for assessing functional status and response to treatment.
- Echocardiography:
- Used to evaluate the impact of COPD on the heart, especially in patients with suspected pulmonary hypertension or right ventricular dysfunction.
- Electrocardiogram (ECG):
- Helps detect cardiac complications such as arrhythmias or right heart strain.
Combining these diagnostic tools allows clinicians to establish a diagnosis of COPD, determine its severity, and formulate an effective treatment plan.
7. Treatment Options
While COPD is a chronic and irreversible condition, various treatment strategies can help manage symptoms, improve quality of life, and slow disease progression. Treatment is tailored to the individual’s symptoms, severity, and overall health.
7.1. Lifestyle Modifications and Supportive Care
Smoking Cessation:
- The Most Critical Intervention:
- Quitting smoking is the single most effective way to slow the progression of COPD. Support options include counseling, nicotine replacement therapy, and prescription medications such as bupropion or varenicline.
- Avoiding Exposure:
- Avoiding secondhand smoke and reducing exposure to environmental pollutants is also essential.
Exercise and Pulmonary Rehabilitation:
- Regular Physical Activity:
- Exercise improves respiratory muscle strength and overall endurance. Pulmonary rehabilitation programs combine exercise training, education, and support to help patients manage their symptoms and improve functional capacity.
- Structured Programs:
- Pulmonary rehabilitation has been shown to improve quality of life and reduce hospitalizations.
Nutritional Support:
- Balanced Diet:
- A healthy diet that is low in sodium and saturated fats helps manage blood pressure and weight.
- Nutritional Counseling:
- For patients with advanced COPD, nutritional counseling can help prevent cachexia (weight loss and muscle wasting).
Vaccinations:
- Preventive Measures:
- Annual influenza vaccinations and pneumococcal vaccines are strongly recommended to prevent respiratory infections that can exacerbate COPD.
7.2. Medications
Medications are central to the management of COPD and are aimed at relieving symptoms, improving airflow, and preventing exacerbations.
Bronchodilators
Bronchodilators help relax the muscles around the airways, improving airflow and reducing breathlessness.
- Short-Acting Bronchodilators (SABAs):
- Examples: Albuterol, levalbuterol.
- Usage: Provide quick relief during acute episodes of dyspnea.
- Long-Acting Bronchodilators (LABAs):
- Examples: Salmeterol, formoterol.
- Usage: Used regularly to maintain open airways and reduce symptoms.
- Anticholinergics:
- Short-Acting (SAMAs): Ipratropium.
- Long-Acting (LAMAs): Tiotropium, aclidinium.
- Mechanism: Block acetylcholine receptors to relax airway smooth muscle.
Inhaled Corticosteroids (ICS)
- Usage:
- Often combined with LABAs in patients with frequent exacerbations or significant inflammation.
- Examples: Fluticasone, budesonide.
- Benefits:
- Reduce airway inflammation and decrease the frequency of exacerbations.
Combination Inhalers
- Fixed-Dose Combinations:
- These inhalers combine bronchodilators and inhaled corticosteroids to provide both rapid relief and long-term control.
- Examples: Fluticasone/salmeterol, budesonide/formoterol.
Phosphodiesterase-4 (PDE-4) Inhibitors
- Example: Roflumilast.
- Mechanism:
- Reduce inflammation by inhibiting the enzyme phosphodiesterase-4, which can help decrease the frequency of exacerbations in severe COPD.
Oxygen Therapy
- Supplemental Oxygen:
- Recommended for patients with significant hypoxemia (low blood oxygen levels). Long-term oxygen therapy can improve survival in patients with severe COPD.
- Monitoring:
- Oxygen saturation is regularly monitored, and therapy is adjusted to maintain levels above 90%.
Antibiotics
- Exacerbation Management:
- Antibiotics are used during acute exacerbations, particularly when bacterial infections are suspected.
- The choice of antibiotic is based on local resistance patterns and patient history.
7.3. Interventional and Surgical Treatments
For patients with advanced COPD who do not respond adequately to medications and lifestyle changes, interventional procedures may be considered.
Bronchoscopic Lung Volume Reduction (BLVR)
- Procedure:
- Minimally invasive techniques such as endobronchial valves, coils, or thermal vapor ablation help reduce lung hyperinflation by collapsing diseased portions of the lung.
- Benefits:
- Improves breathing efficiency and quality of life in selected patients with emphysema.
Lung Volume Reduction Surgery (LVRS)
- Indication:
- LVRS is a surgical option for patients with severe emphysema.
- The procedure involves removing the most diseased portions of the lung to allow the healthier lung tissue to function more efficiently.
- Outcomes:
- LVRS can significantly improve symptoms and exercise capacity in carefully selected patients.
Lung Transplantation
- End-Stage Treatment:
- For patients with end-stage COPD who have exhausted all other treatment options, lung transplantation may be considered.
- Selection Criteria:
- Not all patients are candidates for transplantation; rigorous evaluation is required.
7.4. Emerging Therapies and Research
Research continues to explore novel treatments for COPD, including:
- New Bronchodilators and Anti-inflammatory Agents:
- Ongoing trials are investigating drugs that target specific inflammatory pathways involved in COPD.
- Stem Cell Therapy:
- Experimental approaches aim to repair or regenerate damaged lung tissue.
- Gene Therapy:
- Although still in the early stages, gene therapy may offer future treatment options by addressing genetic predispositions and underlying mechanisms.
- Biologic Agents:
- These are targeted therapies designed to block specific cytokines and inflammatory mediators involved in COPD.
Clinical trials and emerging research are key to understanding and eventually overcoming the limitations of current treatments.
8. Available Support Groups and Resources
Living with COPD can be challenging, both physically and emotionally. Fortunately, numerous support resources are available to help patients and their families cope with the disease.
National Organizations
- American Lung Association (ALA):
- Provides extensive resources on COPD, including educational materials, support groups, and advocacy initiatives.
- COPD Foundation:
- Focuses specifically on COPD education, research funding, and support for patients.
- National Heart, Lung, and Blood Institute (NHLBI):
- Offers information on COPD research, clinical trials, and patient resources.
Local and Online Support Groups
- Mayo Clinic Connect:
- An online community where patients with COPD share their experiences and coping strategies.
- Support Forums on Health Websites:
- Websites like WebMD, MedHelp, and Inspire host discussion boards dedicated to COPD.
- Social Media Groups:
- Facebook and Twitter groups provide peer support, updated research news, and practical advice for managing COPD.
Educational Resources
- Mayo Clinic, Johns Hopkins Medicine, and Cleveland Clinic:
- These reputable institutions offer patient-friendly information on COPD management and treatment options.
- MedlinePlus and CDC:
- Provide reliable, government-sponsored resources on COPD prevention and care.
Connecting with support groups and educational resources is an essential component of managing COPD and improving quality of life.
9. Prognosis
Disease Course and Outcomes
COPD is a chronic, progressive disease. Its prognosis varies depending on the severity at diagnosis, the rate of progression, and the presence of comorbid conditions.
- Mild to Moderate COPD:
- Many patients maintain a relatively good quality of life for years with appropriate treatment and lifestyle modifications.
- Severe COPD:
- As the disease advances, symptoms worsen, and patients may experience frequent exacerbations, declining lung function, and ultimately, respiratory failure.
Factors Affecting Prognosis
Several factors influence the long-term outcomes for individuals with COPD:
- Smoking History:
- Continued smoking accelerates disease progression, while smoking cessation is the most effective intervention to slow the decline.
- Frequency of Exacerbations:
- Frequent exacerbations (acute worsening of symptoms) are associated with a more rapid decline in lung function.
- Lung Function (FEV₁):
- Lower baseline FEV₁ values are predictive of poorer outcomes.
- Comorbidities:
- The presence of other conditions such as cardiovascular disease, diabetes, or osteoporosis can negatively impact prognosis.
- Response to Treatment:
- Patients who adhere to treatment plans and make healthy lifestyle changes tend to have better outcomes.
Survival and Quality of Life
While COPD is not curable, effective management can significantly improve quality of life and survival:
- Oxygen Therapy:
- Long-term oxygen therapy in patients with severe hypoxemia has been shown to improve survival.
- Pulmonary Rehabilitation:
- Participation in rehabilitation programs can enhance exercise capacity and overall well-being.
- Regular Monitoring and Intervention:
- Early detection of complications and timely treatment of exacerbations help maintain a stable disease course.
Prognostic models, such as the BODE index (which incorporates Body mass index, airflow Obstruction, Dyspnea, and Exercise capacity), are used to predict outcomes and guide treatment decisions.
10. Possible Complications
COPD can lead to numerous complications that affect various organ systems. Recognizing these complications early is critical for prompt intervention.
Respiratory Complications
- Exacerbations:
- Acute exacerbations are episodes of sudden worsening of symptoms, often triggered by infections or environmental factors. These events can accelerate the decline in lung function.
- Respiratory Failure:
- In advanced COPD, the lungs may no longer be able to maintain adequate oxygenation, leading to respiratory failure.
- Pulmonary Hypertension and Cor Pulmonale:
- Chronic hypoxia can lead to increased pressure in the pulmonary arteries, which may eventually cause right ventricular hypertrophy (cor pulmonale) and heart failure.
- Lung Infections:
- Increased susceptibility to pneumonia, bronchitis, and other respiratory infections.
Cardiovascular Complications
- Arrhythmias:
- COPD can contribute to abnormal heart rhythms, including atrial fibrillation.
- Heart Failure:
- The strain on the heart due to chronic lung disease may result in heart failure, particularly right-sided failure.
- Increased Risk of Stroke:
- Arrhythmias and impaired oxygenation increase the risk of thromboembolic events such as stroke.
Systemic Complications
- Osteoporosis:
- Chronic inflammation, use of corticosteroids, and reduced physical activity contribute to bone loss.
- Muscle Wasting and Cachexia:
- Advanced COPD may lead to significant weight loss and muscle wasting, affecting overall strength and mobility.
- Anxiety and Depression:
- The chronic nature of COPD and its impact on daily life can lead to mental health issues.
11. Indications for Seeking Medical Attention
Early and prompt medical evaluation is vital for managing COPD and preventing complications. Here are key indicators that you should seek medical attention:
When to Contact Your Healthcare Provider
- Worsening Breathlessness:
- A noticeable increase in shortness of breath during everyday activities or at rest.
- Increased Cough and Sputum Production:
- Especially if the sputum becomes discolored or is accompanied by fever, which may indicate an infection.
- Chest Pain or Tightness:
- Any new or worsening chest discomfort should be evaluated immediately.
- Swelling in the Legs or Ankles:
- This may indicate fluid retention and potential heart failure.
- Dizziness or Fainting:
- Episodes of lightheadedness or syncope can be signs of severe oxygen deprivation or arrhythmia.
- Persistent Fatigue:
- Unexplained tiredness that interferes with daily life.
- Rapid or Irregular Heartbeat:
- Palpitations or a noticeably rapid heart rate, which could signal arrhythmia.
When to Seek Emergency Care
- Severe Chest Pain:
- Especially if accompanied by shortness of breath, sweating, or nausea.
- Sudden, Severe Breathlessness:
- If you experience a dramatic worsening of respiratory symptoms that does not improve with rest.
- Loss of Consciousness:
- Fainting or near-fainting episodes should be evaluated promptly.
- Signs of Acute Respiratory Failure:
- Such as confusion, bluish discoloration of the lips or skin, or a dramatic drop in oxygen saturation.
Immediate medical attention in these scenarios can be life-saving.
12. Preventive Measures
While COPD cannot be cured, there are several preventive strategies that can help slow disease progression and reduce the risk of complications.
Smoking Cessation
- Quit Smoking:
- Since smoking is the primary cause of COPD, cessation is the most effective preventive measure.
- Utilize counseling, nicotine replacement therapies, or prescription medications.
- Avoid Secondhand Smoke:
- Reducing exposure to environmental tobacco smoke is also crucial.
Environmental and Occupational Precautions
- Air Quality:
- Avoid exposure to pollutants, dust, and chemicals. Use protective equipment if you work in high-risk environments.
- Indoor Air Quality:
- Use air purifiers and maintain good ventilation in your home.
Vaccinations
- Influenza Vaccine:
- Annual flu shots can prevent respiratory infections that may exacerbate COPD.
- Pneumococcal Vaccine:
- Prevents pneumonia, a common complication in COPD patients.
- COVID-19 Vaccination:
- Stay up-to-date with COVID-19 vaccinations and boosters as recommended.
Healthy Lifestyle
- Regular Exercise:
- Engage in moderate physical activity to strengthen respiratory muscles and improve overall cardiovascular health.
- Balanced Diet:
- Maintain a diet low in sodium and saturated fats to help control blood pressure and support overall health.
- Weight Management:
- Keeping a healthy weight reduces the burden on the respiratory and cardiovascular systems.
- Stress Reduction:
- Manage stress through mindfulness, counseling, or other relaxation techniques, as stress can worsen COPD symptoms.
Medical Management
- Regular Check-Ups:
- Routine visits to your healthcare provider for monitoring of lung function, blood pressure, and overall health.
- Early Intervention:
- Prompt treatment of respiratory infections and exacerbations can prevent further deterioration.
- Adherence to Medication:
- Taking prescribed medications consistently is vital to maintain lung function and prevent complications.
Patient Education and Support
- Learn About Your Condition:
- Educate yourself using reliable sources such as the American Lung Association, Mayo Clinic, and National Heart, Lung, and Blood Institute (NHLBI).
- Genetic Counseling:
- If you are at risk for COPD due to family history or other factors, consider genetic counseling for more personalized risk assessment.
Implementing these preventive measures can help slow the progression of COPD, reduce the risk of exacerbations, and improve overall quality of life.
13. Conclusion
Chronic Obstructive Pulmonary Disease (COPD) is a complex and progressive lung condition that represents a major public health challenge. Defined by persistent airflow limitation due to chronic inflammation and structural changes in the lungs, COPD encompasses conditions such as chronic bronchitis and emphysema. While smoking is the primary risk factor, environmental exposures, genetic predispositions, and recurrent respiratory infections also play significant roles.
The clinical manifestations of COPD vary from a chronic cough and sputum production to severe dyspnea and exercise intolerance. Early in the disease, many patients remain asymptomatic; however, as COPD progresses, symptoms become more pronounced and can significantly impact daily life. Accurate diagnosis relies on a combination of patient history, physical examination, spirometry, imaging studies, and laboratory tests. In some cases, additional evaluations such as the six-minute walk test and echocardiography are used to assess disease severity and complications.
Management of COPD is multifaceted and includes lifestyle modifications, smoking cessation, pharmacotherapy (bronchodilators, inhaled corticosteroids, PDE-4 inhibitors), and in advanced cases, supplemental oxygen, pulmonary rehabilitation, and even surgical interventions. Emerging therapies continue to be investigated, and participation in clinical trials offers hope for more effective treatments in the future.
Preventive measures, including avoiding tobacco smoke, maintaining a healthy lifestyle, and ensuring regular medical check-ups, are critical to slowing disease progression and improving outcomes. Equally important is the availability of support groups and educational resources, which help patients cope with the emotional and physical challenges of living with COPD.
In summary, while COPD remains a chronic and incurable condition, a proactive, comprehensive approach to management can greatly enhance quality of life and extend survival. Patients, caregivers, and healthcare professionals must work collaboratively to tailor treatment plans, monitor progress, and address complications as they arise. With continued research and public health efforts, the burden of COPD can be reduced, offering hope for improved outcomes for millions of people worldwide.
References
- Mayo Clinic. “Chronic Obstructive Pulmonary Disease (COPD) – Symptoms and Causes.” Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679.
- American Lung Association. “What is COPD?” American Lung Association. Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd.
- National Heart, Lung, and Blood Institute (NHLBI). “COPD.” NHLBI. Retrieved from https://www.nhlbi.nih.gov/health/copd.
- Centers for Disease Control and Prevention (CDC). “COPD.” CDC. Retrieved from https://www.cdc.gov/copd/index.html.
- Vestbo J, Hurd SS, Agustí AG, et al. “Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary.” American Journal of Respiratory and Critical Care Medicine. 2013;187(4):347-365.
- Celli BR, MacNee W, ATS/ERS Task Force. “Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper.” European Respiratory Journal. 2004;23(6):932-946.
- Wedzicha JA, Seemungal TA. “COPD exacerbations: defining their cause and prevention.” The Lancet. 2007;370(9589):786-796.
- Ohar JA, Make BJ, Yawn BP. “Chronic obstructive pulmonary disease in women: epidemiology, clinical manifestations, and diagnosis.” Women’s Health. 2011;7(6):737-750.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). “Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report).” Available at https://goldcopd.org/.
- National Institutes of Health (NIH). “COPD: A Guide for Patients and Their Families.” Retrieved from https://www.nhlbi.nih.gov/health/copd.