Kidney stones are small, hard deposits that form inside your kidneys from minerals and salts. They can cause severe pain and various complications if not properly managed. This article provides an in-depth overview of kidney stones—including their definition, alternative names, causes, common symptoms, diagnostic tests, treatment options, support groups, prognosis, possible complications, indications for seeking medical attention, and preventive measures—with references to credible, up-to-date medical sources.
1. Definition and Alternative Names
1.1 What Are Kidney Stones?
Kidney stones (also known as renal calculi) are hard deposits that form in the kidneys when certain substances in urine—such as calcium, oxalate, and uric acid—crystallize. These stones vary in size from tiny grains to large masses and can remain in the kidney or travel down the urinary tract, causing severe pain and potential complications.
1.2 Alternative Names
Kidney stones are referred to by several alternative names:
- Renal Calculi: Emphasizing their formation within the kidneys.
- Nephrolithiasis: The medical term for kidney stone formation.
- Urinary Stones: A broader term that includes stones formed in the kidneys, ureters, bladder, or urethra.
- Urolithiasis: Refers to the formation of stones anywhere in the urinary system.
Understanding these terms is useful when reading medical literature, as different sources may use one term over another.
2. Causes and Risk Factors
Kidney stones develop when the concentration of stone-forming substances in urine becomes too high and crystallizes. Several factors contribute to stone formation:
2.1 Chemical Imbalances in the Urine
- High Calcium Levels (Hypercalciuria): Excess calcium in urine can combine with oxalate or phosphate to form stones.
- High Oxalate Levels (Hyperoxaluria): Oxalate, found in many foods, can bind with calcium and form calcium oxalate stones—the most common type.
- High Uric Acid Levels (Hyperuricosuria): Uric acid stones can form in people with high uric acid in their urine.
- Low Citrate Levels: Citrate helps prevent stone formation by binding calcium; low levels (hypocitraturia) increase stone risk.
- Low Urine Volume: Inadequate fluid intake leads to concentrated urine, promoting crystallization.
2.2 Dietary Factors
- High Salt Intake: Excess sodium increases calcium excretion in urine.
- High Protein Diet: Especially animal protein can increase uric acid levels and decrease citrate.
- Foods High in Oxalate: Such as spinach, rhubarb, beets, and nuts may contribute to kidney stone formation.
- Inadequate Fluid Intake: Not drinking enough water is a major risk factor.
2.3 Medical Conditions
Certain health conditions predispose individuals to kidney stone formation:
- Hyperparathyroidism: Overactivity of the parathyroid glands increases calcium levels in blood and urine.
- Gout: Elevated uric acid levels can lead to uric acid stones.
- Obesity and Metabolic Syndrome: These conditions are associated with changes in urine pH and stone risk.
- Digestive Diseases: Conditions such as inflammatory bowel disease (IBD), Crohn’s disease, or gastric bypass surgery can lead to increased oxalate absorption.
2.4 Genetics and Family History
A family history of kidney stones significantly increases the risk, suggesting a genetic predisposition to factors such as hypercalciuria or metabolic abnormalities.
2.5 Medications and Supplements
Certain medications (such as diuretics, calcium-based antacids, and some anti-seizure medications) and supplements (excessive vitamin D or calcium supplements) may contribute to kidney stone formation.
2.6 Environmental and Lifestyle Factors
- Climate: Living in hot climates or working in high temperatures increases fluid loss, raising stone risk.
- Sedentary Lifestyle: Physical inactivity can lead to reduced bone turnover and higher urinary calcium.
Understanding these causes and risk factors is essential to both prevent kidney stones and guide treatment strategies.
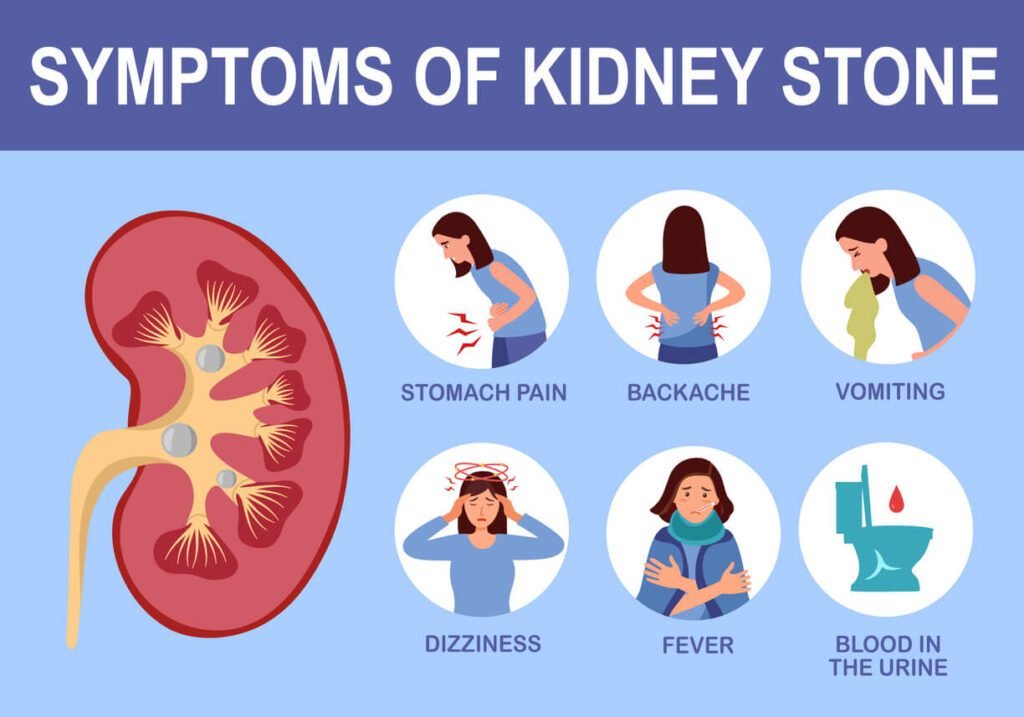
3. Symptoms of Kidney Stones
Kidney stone symptoms vary in severity and depend on the stone’s size, location, and whether it is moving through the urinary tract.
3.1 Pain
The hallmark symptom of kidney stones is pain, which can be intense and debilitating:
- Renal Colic: Characterized by severe, intermittent flank pain that may radiate to the lower abdomen and groin. This pain is often described as one of the most severe experiences.
- Location of Pain: Pain may begin in the back or side (flank pain) and can spread to the lower abdomen, groin, or testicles/labia, depending on the stone’s location in the urinary tract.
- Onset and Duration: Pain can come in waves, with episodes lasting from minutes to several hours. Movement of the stone can lead to sudden changes in pain intensity.
3.2 Urinary Symptoms
Kidney stones can also affect the urinary system, leading to:
- Hematuria: Blood in the urine, which may be visible (gross hematuria) or detected on a lab test (microscopic hematuria). This occurs when stones irritate or scratch the urinary tract.
- Frequency and Urgency: Increased urge to urinate and more frequent urination, especially if the stone is located near the bladder.
- Painful Urination (Dysuria): Discomfort or burning sensation during urination can occur, particularly if a stone is near the ureterovesical junction.
3.3 Gastrointestinal and Other Symptoms
- Nausea and Vomiting: Severe pain can trigger a vasovagal response, leading to nausea and vomiting.
- Fever and Chills: Although kidney stones themselves do not cause fever, fever may indicate an associated infection (such as pyelonephritis), which requires urgent treatment.
- Cloudy or Foul-Smelling Urine: In some cases, urinary tract infection can accompany kidney stones, altering the urine’s appearance and odor.
3.4 Variability in Symptoms
- Small Stones: May pass without causing significant pain or symptoms.
- Large Stones: More likely to cause severe pain, urinary obstruction, and complications.
- Stone Location: Stones located in the kidney may cause mild discomfort, while those that have moved into the ureter typically cause more intense pain.
Overall, the severity of symptoms correlates with the size, location, and movement of the stone, as well as any complications that arise.
4. Diagnostic Exams and Tests
Accurate diagnosis of kidney stones involves a combination of clinical evaluation, laboratory tests, and imaging studies.
4.1 Medical History and Physical Examination
- Detailed History: Your healthcare provider will ask about the onset, duration, and character of your pain, urinary symptoms, and any associated nausea, vomiting, or fever. A family history of kidney stones or related conditions is also important.
- Physical Examination: A focused examination of the abdomen and flank may reveal tenderness. In some cases, a digital rectal or pelvic examination is performed.
4.2 Laboratory Tests
Several laboratory tests help confirm the diagnosis and assess potential complications:
- Urinalysis: A urine sample is analyzed for hematuria (blood), crystals, and signs of infection. The presence of blood or crystals (calcium oxalate, uric acid) supports the diagnosis of kidney stones.
- Blood Tests: Blood tests may include:
- Serum Creatinine and Blood Urea Nitrogen (BUN): To evaluate kidney function.
- Electrolytes and Calcium Levels: Abnormal levels can indicate underlying metabolic disorders.
- Urine Culture: If an infection is suspected.
4.3 Imaging Studies
Imaging is critical in locating and sizing the stone and determining its impact on the urinary tract:
- Non-Contrast Helical CT Scan: Considered the gold standard for kidney stone detection. It provides detailed images, allowing for accurate stone localization, measurement, and detection of associated hydronephrosis (swelling of the kidney due to obstruction).
- Ultrasound: Particularly useful in pregnant patients or when radiation exposure is a concern. While ultrasound is less sensitive than CT for small stones, it can detect larger stones and signs of obstruction.
- Plain Abdominal X-ray (KUB): Can detect radiopaque stones (stones that are visible on X-ray), such as calcium stones. However, it may miss radiolucent stones, such as uric acid stones.
- Intravenous Pyelogram (IVP): An older imaging technique that uses contrast dye to visualize the urinary tract. It is now less commonly used due to advances in CT technology.
4.4 Additional Diagnostic Evaluations
- Stone Analysis: If a stone is passed or surgically removed, it can be analyzed in a laboratory to determine its composition. This information is vital for tailoring preventive strategies.
- Metabolic Evaluation: In patients with recurrent kidney stones, a 24-hour urine collection may be performed to measure levels of stone-forming substances (calcium, oxalate, uric acid) and inhibitors (citrate) to guide long-term management.
5. Treatment Options
Treatment of kidney stones depends on the stone’s size, location, composition, and the severity of symptoms. Management can range from conservative measures to surgical interventions.
5.1 Conservative Management and Medical Therapy
For many patients, especially those with small stones, conservative management is the first line of treatment.
5.1.1 Hydration
- Increased Fluid Intake: Drinking plenty of water (aiming for 2.5 to 3 liters per day) helps dilute the urine and promote stone passage.
- Oral Fluids: Along with water, lemonade or other citrus drinks can be beneficial due to the citrate content, which helps inhibit stone formation.
5.1.2 Pain Management
- Analgesics: Over-the-counter pain relievers such as NSAIDs (ibuprofen) or acetaminophen are commonly used.
- Stronger Medications: In cases of severe pain, prescription opioids may be necessary.
- Adjunctive Therapies: Heat application (such as a heating pad) and rest may help relieve discomfort.
5.1.3 Medical Expulsive Therapy
- Alpha-Blockers: Medications such as tamsulosin can relax the muscles in the ureter, facilitating the passage of stones. They are particularly useful for stones located in the distal ureter.
- Calcium Channel Blockers: Sometimes used as an alternative to alpha-blockers.
5.1.4 Dietary Modifications
- Low Sodium Diet: Reducing salt intake helps decrease urinary calcium excretion.
- Reduced Animal Protein: A high-protein diet can increase stone risk by raising uric acid levels.
- Balanced Calcium Intake: Contrary to outdated advice, a normal calcium intake is important. Too little dietary calcium can increase oxalate absorption, leading to calcium oxalate stones.
- Limiting Oxalate-Rich Foods: In patients prone to calcium oxalate stones, reducing foods high in oxalate (e.g., spinach, nuts) may be beneficial.
- Citrate Supplements: Potassium citrate can help prevent stone formation by binding to calcium.
5.2 Interventional and Surgical Treatments
When conservative management fails or complications develop, more invasive procedures may be necessary.
5.2.1 Extracorporeal Shock Wave Lithotripsy (ESWL)
- Procedure: ESWL uses shock waves to break kidney stones into smaller fragments that can pass through the urinary tract.
- Indications: Best suited for stones smaller than 2 cm located in the kidney or upper ureter.
- Benefits: Minimally invasive and usually performed on an outpatient basis.
- Limitations: Less effective for very large stones or stones composed of hard substances like cystine.
5.2.2 Ureteroscopy
- Procedure: A small flexible scope is inserted through the urethra and bladder into the ureter to locate the stone. Once identified, a laser is used to fragment the stone.
- Indications: Effective for stones in the ureter, particularly if ESWL is not suitable.
- Recovery: Typically requires a short hospital stay with a ureteral stent placed to facilitate urine flow during healing.
5.2.3 Percutaneous Nephrolithotomy (PCNL)
- Procedure: This minimally invasive surgery involves making a small incision in the back and inserting a scope directly into the kidney to remove large stones.
- Indications: Typically used for stones larger than 2 cm or for complex stone burdens.
- Recovery: Patients usually stay in the hospital for a few days after the procedure.
5.2.4 Open or Laparoscopic Surgery
- Procedure: Reserved for cases where other methods are unsuccessful or if anatomical abnormalities require correction.
- Indications: Rarely used but may be necessary for very large, complex stones.
- Recovery: Open surgery has a longer recovery time compared to minimally invasive procedures.
5.3 Adjunctive Therapies and Preventive Medications
5.3.1 Medications to Prevent Recurrence
- Thiazide Diuretics: Can reduce urinary calcium levels.
- Potassium Citrate: Helps increase urinary citrate, a natural inhibitor of stone formation.
- Allopurinol: Used in patients with high uric acid levels to reduce the formation of uric acid stones.
- Magnesium Supplements: May help prevent calcium oxalate stone formation.
5.3.2 Follow-Up and Monitoring
After initial treatment, follow-up care is crucial:
- Imaging Studies: Repeating ultrasound or CT scans to confirm stone passage or identify residual fragments.
- 24-Hour Urine Analysis: To assess for metabolic abnormalities that could predispose to recurrence.
- Regular Medical Appointments: Ongoing monitoring by a healthcare provider helps adjust treatment plans and prevent new stone formation.
6. Available Support Groups and Resources
Dealing with kidney stones can be physically and emotionally challenging. Fortunately, there are many support groups and resources available to help patients manage their condition.
6.1 National Organizations
- American Urological Association (AUA): Offers guidelines, patient education, and support resources for those with kidney stones.
- National Kidney Foundation (NKF): Provides information on kidney stone prevention, treatment, and long-term kidney health.
- Urology Care Foundation: The official foundation of the AUA, offering patient resources, educational materials, and support networks.
6.2 Online Communities and Forums
- MedlinePlus and Healthline: Both provide articles and patient-friendly guides on kidney stones.
- Patient Forums: Websites such as KidneyStoners.com and various Reddit communities (e.g., r/kidneystones) offer platforms for patients to share experiences, advice, and support.
- Social Media Groups: Facebook and other social networks host groups dedicated to individuals with kidney stones, where members share tips on diet, pain management, and lifestyle changes.
6.3 Local Support and Counseling
- Hospital Support Groups: Many hospitals and urology clinics offer support groups where patients can meet others facing similar challenges.
- Nutritional Counseling: Registered dietitians specialized in kidney health can offer personalized dietary advice.
- Counseling Services: Chronic pain and recurring health issues can affect mental health; professional counseling or therapy may be beneficial.
6.4 Educational Materials
- Books and Pamphlets: Numerous books on kidney stones offer comprehensive overviews of the condition, including self-care and prevention strategies.
- Webinars and Workshops: Many organizations host webinars and live workshops that provide the latest information on kidney stone management and prevention.
7. Prognosis and Long-Term Outlook
7.1 Prognosis
The overall prognosis for kidney stones depends on several factors:
- Stone Size and Location: Smaller stones often pass on their own with adequate hydration, while larger stones may require intervention.
- Underlying Causes: Metabolic disorders that predispose individuals to stone formation may require long-term management to prevent recurrence.
- Treatment Response: Timely diagnosis and effective treatment can relieve symptoms and prevent complications, improving the prognosis.
7.2 Recurrence
- High Recurrence Rate: Kidney stones have a high recurrence rate—up to 50% of patients may develop another stone within 5–10 years.
- Preventive Strategies: Adherence to preventive measures, including dietary modifications, medications, and regular follow-up, can significantly reduce the likelihood of recurrence.
7.3 Impact on Quality of Life
- Pain and Discomfort: Acute episodes of renal colic can be excruciating, often leading to emergency department visits and hospitalizations.
- Work and Daily Activities: Frequent stone episodes may lead to time off work, reduced productivity, and a general decline in quality of life.
- Long-Term Complications: Recurrent stones can cause chronic kidney disease, infections, and even permanent damage to the urinary tract if not managed properly.
7.4 Advancements in Management
Ongoing research and technological advances continue to improve outcomes for patients with kidney stones:
- Innovative Imaging: New imaging techniques allow for more accurate detection and monitoring of stones.
- Improved Surgical Techniques: Advances in minimally invasive procedures such as ureteroscopy and PCNL have reduced recovery times and improved stone clearance rates.
- Better Metabolic Evaluation: Enhanced understanding of metabolic risk factors has led to more personalized preventive strategies.
Overall, with modern treatment and preventive strategies, many patients can lead normal, active lives, though the risk of recurrence remains a challenge.
8. Possible Complications
Kidney stones can lead to several complications if not treated promptly or managed effectively.
8.1 Urinary Tract Obstruction
- Partial or Complete Obstruction: A stone lodged in the ureter may block the flow of urine, leading to hydronephrosis (swelling of the kidney) and pain.
- Infection Risk: Urinary stasis from an obstruction increases the risk of urinary tract infections (UTIs) and, in severe cases, pyelonephritis (kidney infection).
8.2 Infection
- Sepsis: An untreated urinary tract infection in the presence of kidney stones can progress to sepsis, a life-threatening systemic response to infection.
- Chronic Infections: Recurrent infections can damage the kidney and impair its function over time.
8.3 Kidney Damage
- Hydronephrosis: Persistent obstruction can cause pressure buildup and swelling in the kidney, eventually leading to kidney damage.
- Chronic Kidney Disease (CKD): Repeated stone episodes and associated infections can gradually reduce kidney function, potentially leading to CKD.
8.4 Bleeding
- Hematuria: Stones can irritate or scratch the lining of the urinary tract, leading to blood in the urine.
- Severe Bleeding: In some cases, the irritation may cause significant bleeding, which can be distressing and require medical attention.
8.5 Stone Recurrence
- Recurrent Stone Formation: Without proper preventive measures, kidney stones tend to recur, leading to repeated episodes of pain and possible complications.
8.6 Invasive Procedures Complications
- Surgical Risks: Procedures such as ESWL, ureteroscopy, and PCNL carry risks including infection, bleeding, injury to surrounding tissues, and anesthesia-related complications.
- Residual Fragments: Incomplete stone clearance can lead to residual fragments, which may serve as a nidus for new stone formation.
9. Indications for Seeking Medical Attention
Knowing when to seek medical help is crucial for preventing complications and ensuring prompt treatment. You should contact your healthcare provider or visit an emergency room if you experience:
9.1 Severe, Unrelenting Pain
- Intensity: Pain that is severe, persistent, and unresponsive to over-the-counter pain relievers.
- Location: Flank pain that radiates to the lower abdomen or groin, which may indicate that a stone is moving through the ureter.
- Action: If pain is overwhelming or worsening, seek immediate evaluation.
9.2 Signs of Infection
- Fever and Chills: High temperature, chills, or shaking can be signs of a urinary tract infection or kidney infection.
- Cloudy or Foul-Smelling Urine: These changes in urine appearance may indicate an infection.
- Action: Prompt medical attention is essential to prevent complications such as sepsis.
9.3 Hematuria
- Visible Blood in Urine: While some blood may be present with kidney stones, significant or persistent hematuria should be evaluated.
- Action: Consult a healthcare provider for assessment and appropriate treatment.
9.4 Inability to Urinate
- Urinary Retention: If you’re unable to pass urine or feel an urgent need to urinate with little output, it may indicate an obstruction.
- Action: Seek emergency care to relieve the blockage.
9.5 Signs of Kidney Infection or Failure
- Flank Pain with Fever: Accompanied by nausea or vomiting, these symptoms can suggest pyelonephritis.
- Decreased Urine Output: A reduction in urine production, along with swelling or weight gain, could indicate impaired kidney function.
- Action: Immediate evaluation is necessary.
9.6 Other Concerning Symptoms
- Nausea and Vomiting: Persistent vomiting may lead to dehydration and worsen kidney stone symptoms.
- General Malaise and Weakness: Severe weakness or dizziness, especially when combined with pain or fever, warrants prompt assessment.
- Action: Contact your healthcare provider for guidance.
10. Preventive Measures and Self-Care
Preventing kidney stones involves a combination of lifestyle changes, dietary modifications, and ongoing medical care.
10.1 Hydration
- Drink Plenty of Fluids: Aim for at least 2.5 to 3 liters of water per day to keep urine diluted.
- Citrus Juices: Lemonade or orange juice contains citrate, a natural inhibitor of stone formation.
10.2 Dietary Modifications
- Reduce Sodium Intake: A low-salt diet can help reduce calcium excretion in the urine.
- Balanced Calcium Intake: Adequate dietary calcium is important; low calcium intake can increase oxalate absorption.
- Limit Oxalate-Rich Foods: Foods such as spinach, rhubarb, nuts, and chocolate may need to be limited in patients prone to calcium oxalate stones.
- Moderate Animal Protein: High consumption of animal protein may increase stone risk by raising uric acid levels.
- Increase Dietary Citrate: In addition to citrus juices, foods rich in citrate may help reduce stone formation.
10.3 Medications and Supplements
- Thiazide Diuretics: May be prescribed to reduce urinary calcium levels in recurrent stone formers.
- Potassium Citrate Supplements: Help increase urinary citrate and prevent stone formation.
- Allopurinol: In cases with high uric acid levels, allopurinol can reduce the risk of uric acid stones.
- Magnesium Supplements: May help prevent calcium oxalate stone formation in some individuals.
10.4 Lifestyle Changes
- Maintain a Healthy Weight: Obesity is associated with an increased risk of kidney stones.
- Regular Physical Activity: Moderate exercise helps improve overall health and may reduce the risk of stone formation.
- Avoid Dehydration: Especially in hot weather or during exercise, always ensure proper hydration.
10.5 Regular Follow-Up
- Medical Monitoring: Regular check-ups and urine analyses help detect early signs of stone formation or metabolic abnormalities.
- Imaging: Periodic imaging studies may be recommended in patients with recurrent stones.
- Stone Analysis: If a stone passes or is removed, having it analyzed can guide future preventive strategies.
10.6 Education and Support
- Patient Education: Learning about kidney stones, triggers, and preventive measures empowers patients to manage their condition effectively.
- Support Groups: Joining support groups or online communities can provide encouragement, practical tips, and a sense of camaraderie.
11. References and Credible Medical Sources
Below is a list of key references that support the information in this article. These sources are widely regarded as authoritative and current:
Mayo Clinic: “Kidney Stones – Symptoms & Causes.”
https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755National Kidney Foundation: Information on kidney stones, prevention, and treatment.
https://www.kidney.org/atoz/content/kidneystonesMedlinePlus (U.S. National Library of Medicine): “Kidney Stones.”
https://medlineplus.gov/kidneystones.htmlJohns Hopkins Medicine: “Kidney Stones: Diagnosis & Treatment.”
https://www.hopkinsmedicine.org/health/conditions-and-diseases/kidney-stonesCleveland Clinic: “Kidney Stones Overview.”
https://my.clevelandclinic.org/health/diseases/14802-kidney-stonesAmerican Urological Association (AUA): Guidelines and patient education resources on kidney stones.
https://www.auanet.org/education/kidney-stonesNational Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Detailed information on kidney stones.
https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stonesUpToDate: Evidence-based clinical information on kidney stone management (subscription required).
Healthline and WebMD: Reliable articles on kidney stone symptoms, diagnosis, and treatment.
Peer-Reviewed Journals:
- Türk C, et al. “Kidney Stones: Pathogenesis, Diagnosis, and Management.” Urolithiasis Research. 2024.
- Scales CD Jr, et al. “Epidemiology of Kidney Stones.” Clinical Journal of the American Society of Nephrology. 2012;7(2):365-371.